Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Decreased acetabular and femoral Anteversion, a Cause of Impingement, slipped femoral epiphysis and Osteoarthritis of the Hip
© Prof. Dr. med. Dietrich Tönnis, Dr. med. Achim Heinecke
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
 The human hip joint has been investigated for a long time mainly by the antero-posterior radiography, to a smaller degree by the lateral "faux-profil" view described by Lequesne and de Seze (Fig. 1).
The human hip joint has been investigated for a long time mainly by the antero-posterior radiography, to a smaller degree by the lateral "faux-profil" view described by Lequesne and de Seze (Fig. 1).
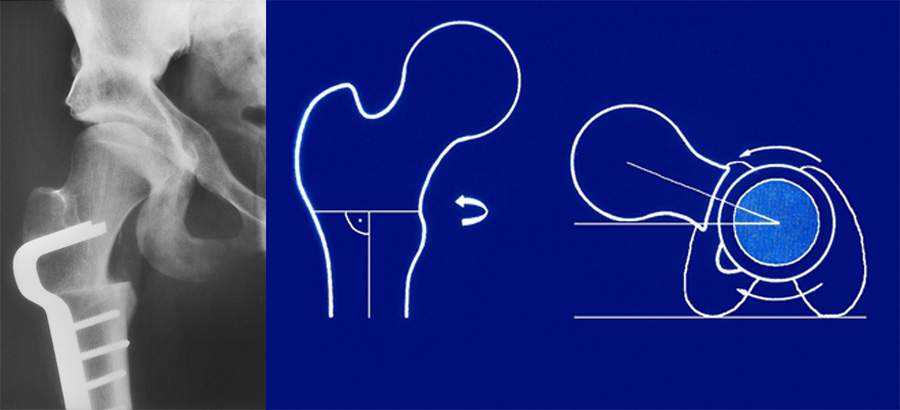
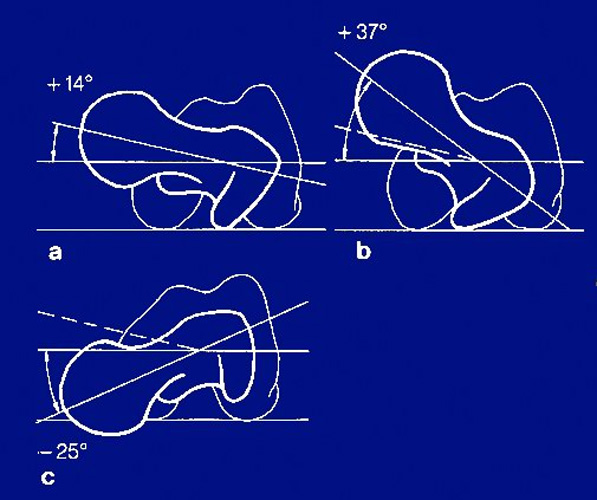 The third plane, the horizontal, shows us the torsion of the femur and the anteversion of the femoral neck. It can be increased or decreased to a pathological degree (Fig. 2).
The third plane, the horizontal, shows us the torsion of the femur and the anteversion of the femoral neck. It can be increased or decreased to a pathological degree (Fig. 2).
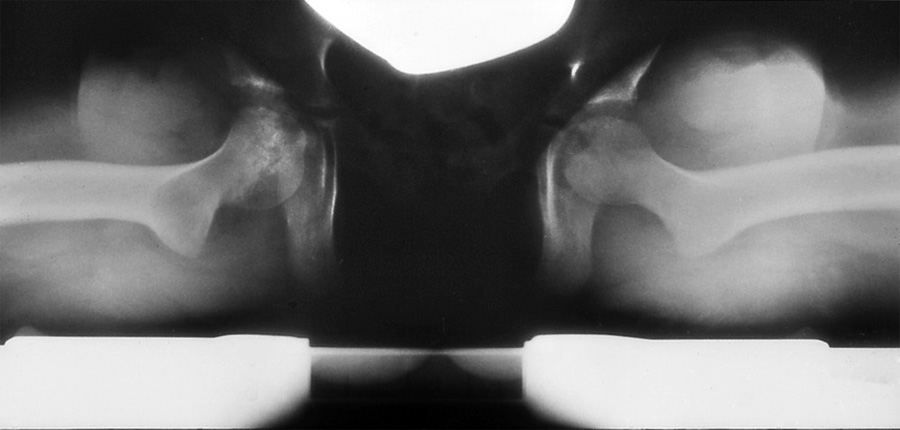
 We evaluate it by the biplane radiography of Rippstein and Müller (Fig. 3).
We evaluate it by the biplane radiography of Rippstein and Müller (Fig. 3).
 An increased anteversion (Fig. 4) was found in young girls who frequently show a marked gait. But Suisse and American authors found, that in about 90% the spontaneous development of the femoral ante-version comes to normal values. Investigators have also tried to find out whether increased femoral anteversion is causing osteoarthrosis of the hip or not. Some found evidence, but others did not.
An increased anteversion (Fig. 4) was found in young girls who frequently show a marked gait. But Suisse and American authors found, that in about 90% the spontaneous development of the femoral ante-version comes to normal values. Investigators have also tried to find out whether increased femoral anteversion is causing osteoarthrosis of the hip or not. Some found evidence, but others did not.
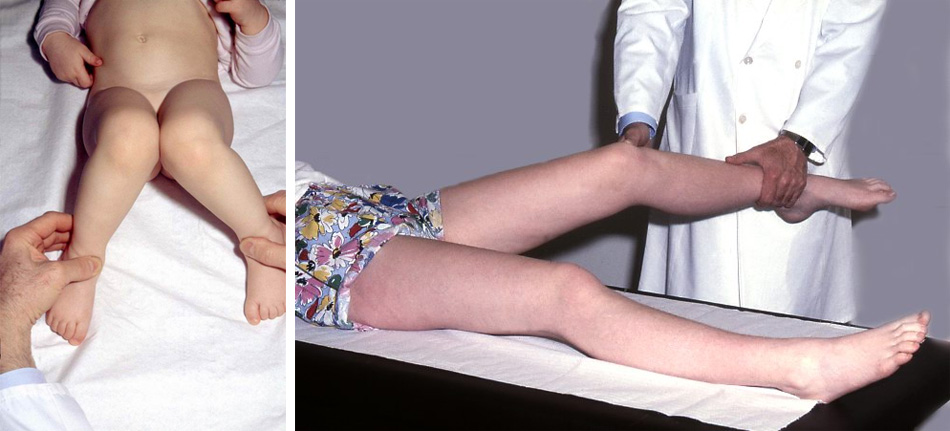
 Decreased femoral anteversion (Fig. 5) so far has not got much attention. Crane described in 1959, that in decreased anteversion there is a limited internal rotation and increased external rotation of the hip with a toeing-out gait.
Decreased femoral anteversion (Fig. 5) so far has not got much attention. Crane described in 1959, that in decreased anteversion there is a limited internal rotation and increased external rotation of the hip with a toeing-out gait.
In his material this was already found in the first year of life and in a number of cases it became worse with age. Similar findings were published by Pitkow in 1975.
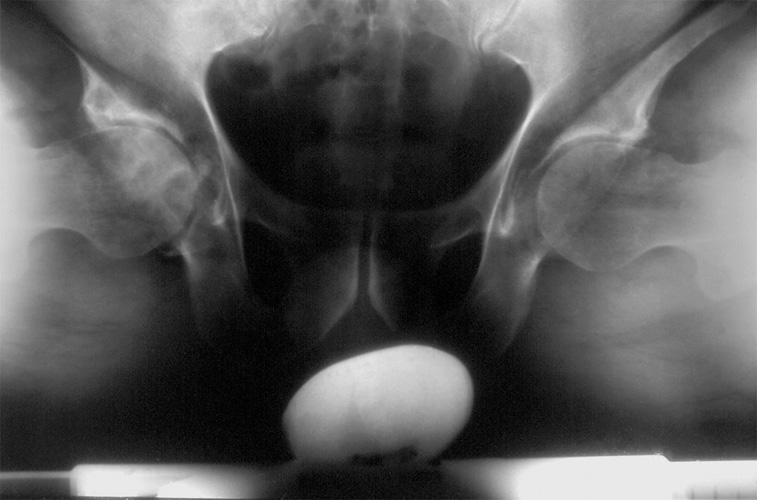
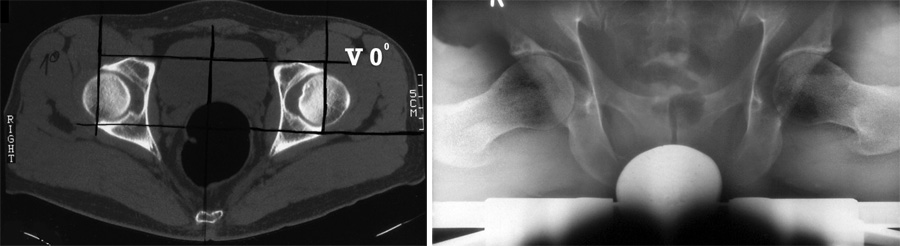
 We came to this diagnosis, when we saw two children with so called "external rotation contractures" of the hips. The first one was a 13 year old girl (Fig. 6). The grandmother and another member of the family showed the same syndrome.
We came to this diagnosis, when we saw two children with so called "external rotation contractures" of the hips. The first one was a 13 year old girl (Fig. 6). The grandmother and another member of the family showed the same syndrome.
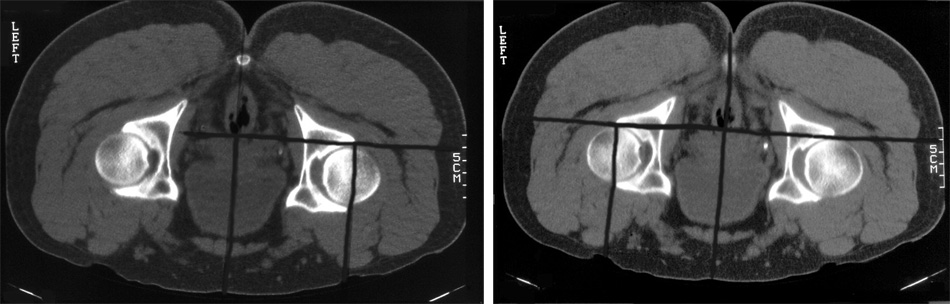
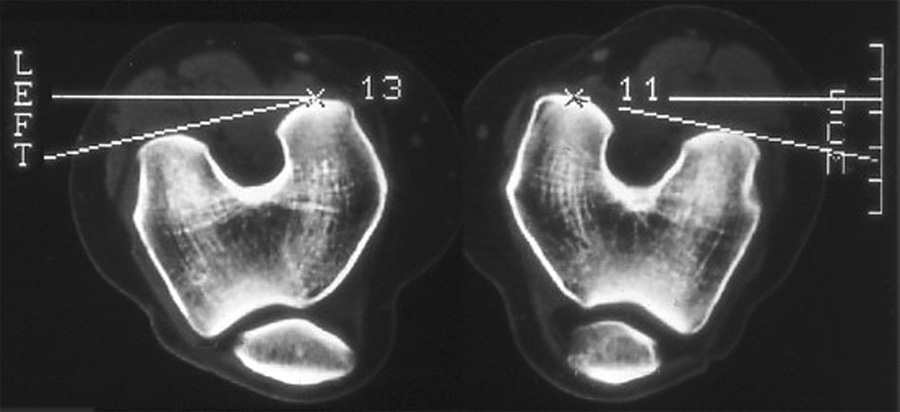
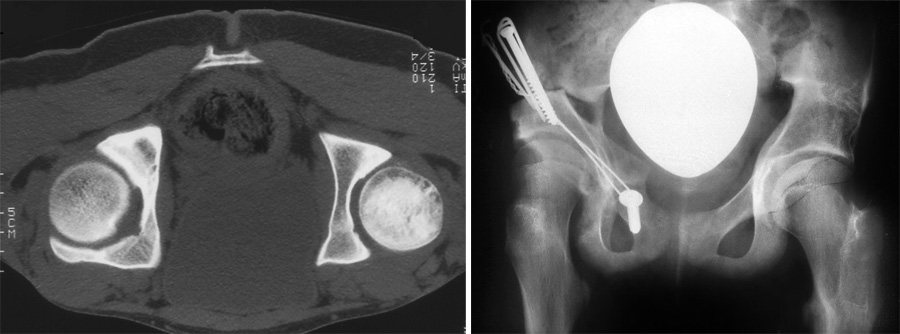
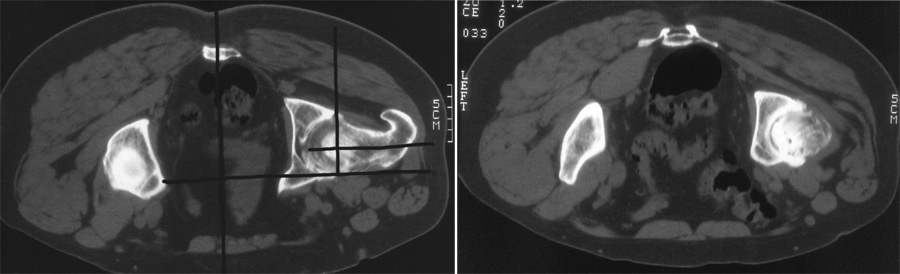
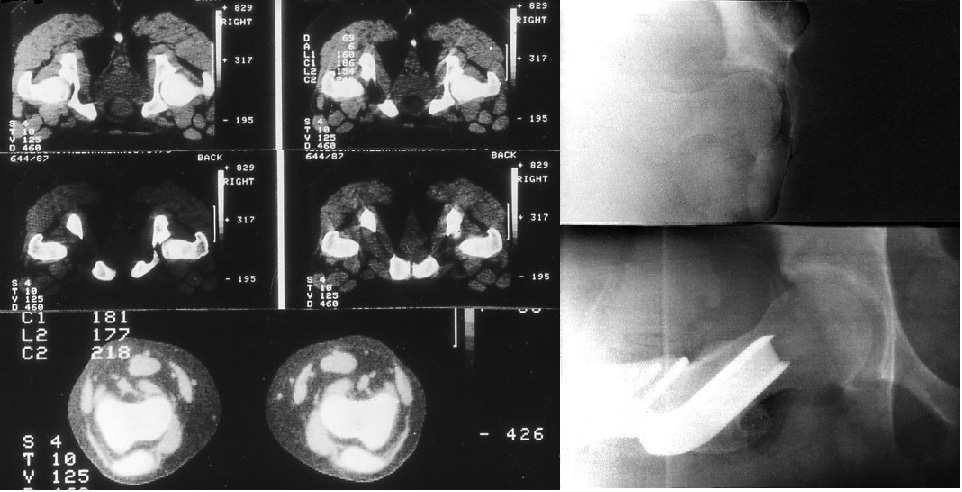 In the CT (Fig. 7) of an early technique the femoral anteversion was zero, in the radiography of Rippstein as well. During the operation we rotated the femoral neck so far that the internal rotation was 20° higher than the external. That is important The gait was normal then and pain relieved.
In the CT (Fig. 7) of an early technique the femoral anteversion was zero, in the radiography of Rippstein as well. During the operation we rotated the femoral neck so far that the internal rotation was 20° higher than the external. That is important The gait was normal then and pain relieved.
 This 6 year old child also shows the knees externally rotated and the lower legs internally as a compensation (Fig. 8).
This 6 year old child also shows the knees externally rotated and the lower legs internally as a compensation (Fig. 8).
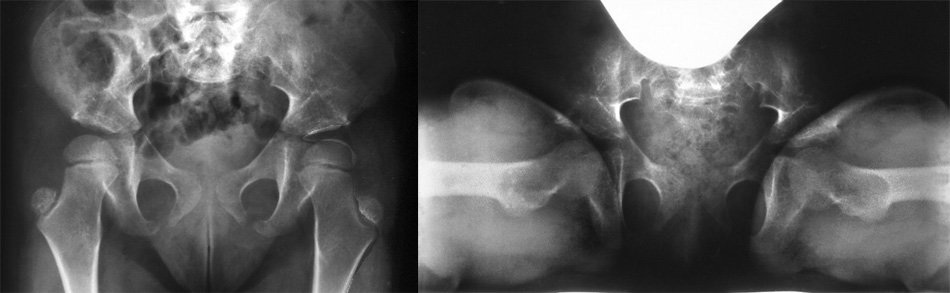
In the ap pelvic picture the greater trochanter of both hips is standing so exactly lateral, that there cannot be much anteversion. In the right picture it seems, that there is a retroversion of the proximal femoral epiphysis (Fig. 9).
 In both legs an anterior femoral rotation osteotomy and an internally rotating tibiaosteotomy were performed (Fig. 10).
In both legs an anterior femoral rotation osteotomy and an internally rotating tibiaosteotomy were performed (Fig. 10).

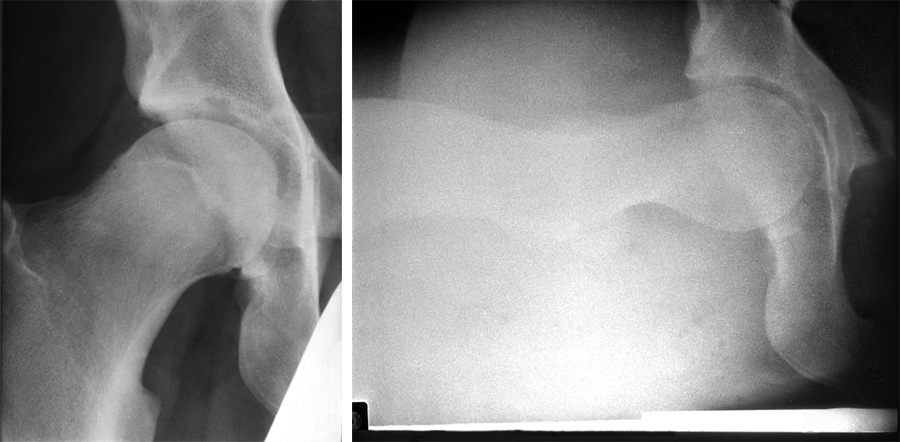
This 25 year old lady had pain in her hip joints (Fig. 11). But there is no hip dysplasia. Here internal rotation is limited, the external increased as in beginning arthrosis. The radiography of Rippstein and Müller shows that there is almost no femoral anteversion in both hips.
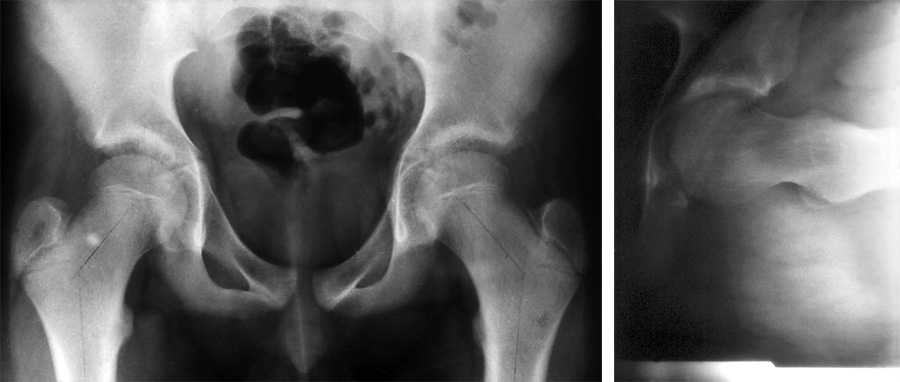
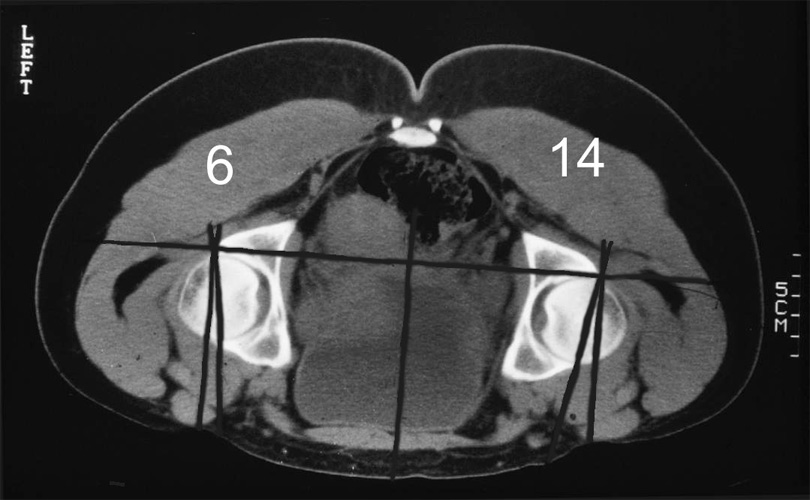
That is the pelvis of a 12 year old boy (Fig. 12). The radiography does not give us a diagnosis. Only the fact, that the femoral necks and the greater trochanter are seen without any rotation may be a hint. But this hint can only be detected when the knees are not rotated externally during radiography. Femoral anteversion here was also zero as you see at the right picture.
When you know this syndrome, you detect it quite frequently, especially in men. In a first investigation in 1991 we had collected 59 patients, 111 joints. The age ranged from below 5 years to 55.
The range of femoral internal and external rotation we measure at 45° flexion to obtain a mean rotation value between zero and 90° of flexion, which have different values (Fig. 13).
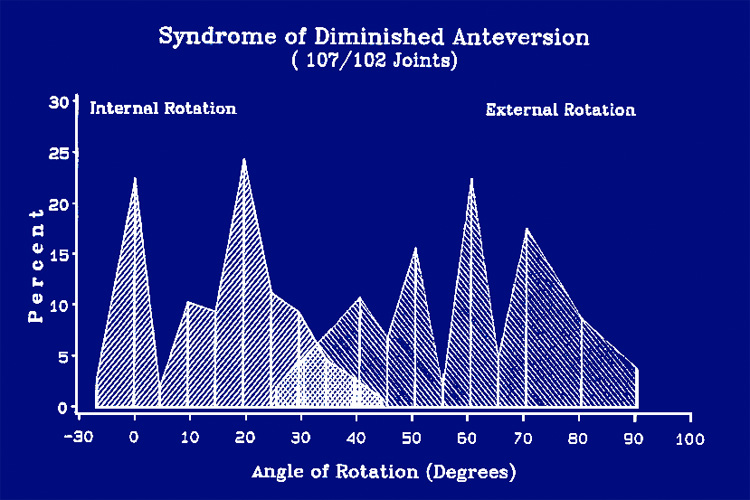 The graph in Fig. 14 shows the range of rotation in these patients. The internal rotation goes down to zero in severe cases and the external rotation rises to more than the double of the internal. But when osteoarthrosis begins, the range gets smaller.
The graph in Fig. 14 shows the range of rotation in these patients. The internal rotation goes down to zero in severe cases and the external rotation rises to more than the double of the internal. But when osteoarthrosis begins, the range gets smaller.
Inguinal region |
55 |
Knee joint (in addition) |
4 |
Patella |
10 |
Illiosacral and gluteal pain |
4 |
Pain was localized mainly at the inguinal region, but frequently and sometimes only at the knee region and specially at the patella (Tab. 1). This is something to remember. The patella then is lateralized and deformed to Wibergs grades 2 to 4 and sometimes dislocates. The tibial tuberosity then should be placed medially.
In some patients the femoral anteversion was not decreased, but the range of movement was changed. We were not able to explain it. Later we discovered, that a retroverted acetabulum can also be responsible for a decreased internal rotation, when it is combined with a normal femoral anteversion. The acetabulum itself has different degrees of anteversion and may be responsible alone for toeing in and out.
Either both, femoral neck and acetabulum have a pathological anteversion, or one has a pathological decreased angle and the other compensates it with a higher angle.
Some years later, when measuring of the anteversion by computer tomographies had made further progress by computer tomographies and when we had collected sufficient material, we made a new investigation of 350 hips in 181 patients. In the CT evaluation a number of special requirements have shown up and orthopaedic surgeons and radiologists should be informed about them (see special article).
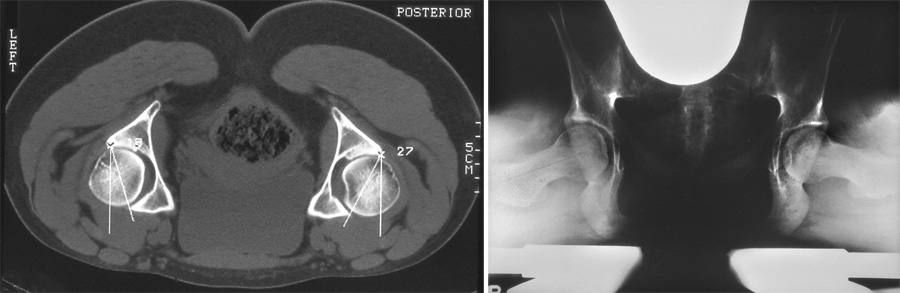
1. As recommended by Visser, the images should be made with the patient in prone position to keep the pelvis in an anatomical position and to avoid a pelvic tilt, which changes the degrees of acetabular anteversion. The feet are slightly supported and lying parallel.
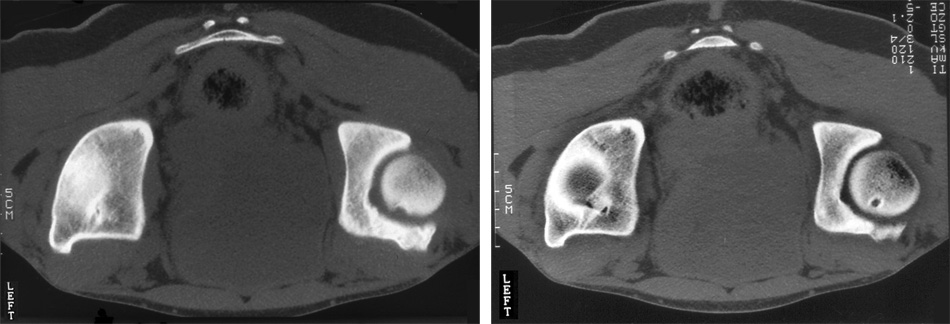
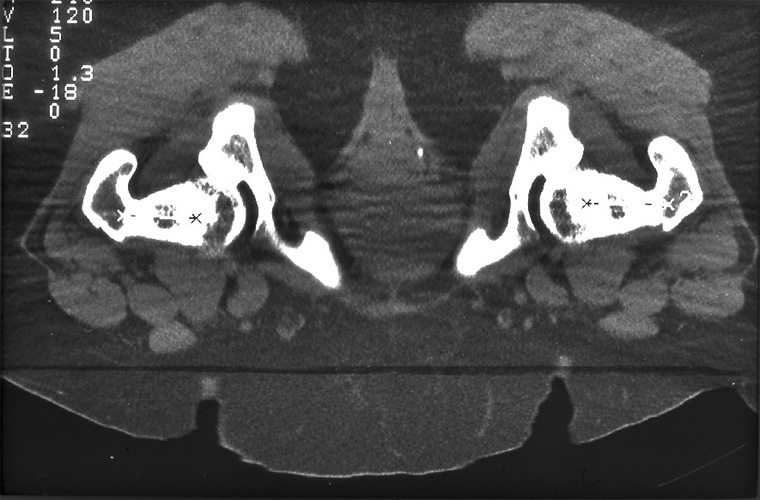
2. The hips should be placed and checked to lie at the same level, and not one more distal than the other, as you see it in the tomographies of Fig. 15.
 3. For the acetabular anteversion, as measured by the CT, the base line is the sagittal plane. The best method is to draw a line midway between the two halves of the pelvis. On each side, a parallel line is drawn, beginning at the posterior margin of the acetabulum. The anteversion angle is then measured between this line and a tangential line to the anterior and posterior acetabular margins (Fig. 16). Our patients, as you see, are now lying prone now.
3. For the acetabular anteversion, as measured by the CT, the base line is the sagittal plane. The best method is to draw a line midway between the two halves of the pelvis. On each side, a parallel line is drawn, beginning at the posterior margin of the acetabulum. The anteversion angle is then measured between this line and a tangential line to the anterior and posterior acetabular margins (Fig. 16). Our patients, as you see, are now lying prone now.
4. Another problem is: at which level of the tomographies of the femoral head should the anteversion angle be measured ? Most authors prefer the level were the femoral head has its largest diameter. But the acetabulum from its roof to the lower margin usually decreases in anteversion.
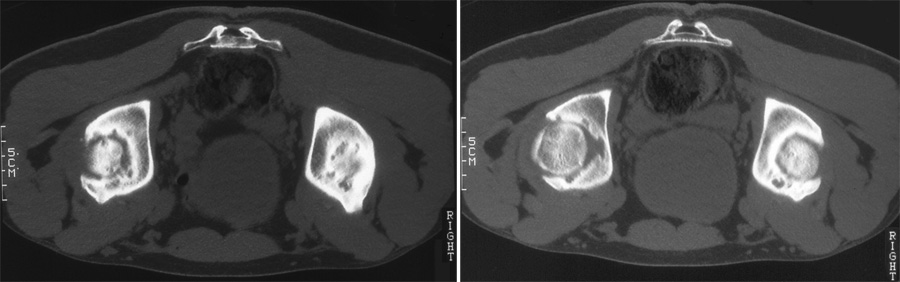
 This you can see at Fig. 17 when you compare the left and the right picture. At the left tomography we find a slight retroversion of the left acetabulum and the anterior margin of the joint is quite long and congruent. At the lower hip the congruence diminishes from the left to the right picture and this increases even more below in Fig. 18. There is almost no acetabular rim any more.
This you can see at Fig. 17 when you compare the left and the right picture. At the left tomography we find a slight retroversion of the left acetabulum and the anterior margin of the joint is quite long and congruent. At the lower hip the congruence diminishes from the left to the right picture and this increases even more below in Fig. 18. There is almost no acetabular rim any more.
Our criterion therefore is: we should measure acetabular anteversion there, where the limitation of internal rotation is caused and impingement takes place. That must be the level, where the femoral head is still enclosed by a congruent and sufficiently long anterior margin.
Anteversion increases in deeper levels of tomography. When measured here – it would be higher.
 The femoral anteversion is measured distally by the transverse knee axis as indicated by a tangential line to the femoral condyles. They should be fully present in the level which is chosen (Fig. 19).
The femoral anteversion is measured distally by the transverse knee axis as indicated by a tangential line to the femoral condyles. They should be fully present in the level which is chosen (Fig. 19).
 The second line should be the axis of the femoral neck. To measure it in the horizontal plane, we have to get a summation picture of all the different scans 3 mm as seen in Fig. 20.
The second line should be the axis of the femoral neck. To measure it in the horizontal plane, we have to get a summation picture of all the different scans 3 mm as seen in Fig. 20.
 This is also necessary because the upper part of the femoral neck is very slim at the trochanteric fossa. Measuring only here, would therefore lead to a more decreased angle (Fig. 21).
This is also necessary because the upper part of the femoral neck is very slim at the trochanteric fossa. Measuring only here, would therefore lead to a more decreased angle (Fig. 21).
 For drawing the axis, one point should lie in the midst of the femoral neck, not at the trochanter, and the other in the center of the femoral head. The base line for the measurements here is a rectangular line to the sagittal plane midline of the pelvis (Fig. 22).
For drawing the axis, one point should lie in the midst of the femoral neck, not at the trochanter, and the other in the center of the femoral head. The base line for the measurements here is a rectangular line to the sagittal plane midline of the pelvis (Fig. 22).
 6. When the feet are lying parallel and there is an external tibial torsion, then the knees will be seen internally rotated as shown here. This angle has then to be added to the angle of the femoral neck. If there is an internal tibial torsion, the knees will appear rotated externally and this angle has to be deducted from the femoral neck angle (Fig. 23).
6. When the feet are lying parallel and there is an external tibial torsion, then the knees will be seen internally rotated as shown here. This angle has then to be added to the angle of the femoral neck. If there is an internal tibial torsion, the knees will appear rotated externally and this angle has to be deducted from the femoral neck angle (Fig. 23).
These measurements we have to compare with the range of internal rotation before and during the operation.
| Grade | Range | Degrees |
| -3 | < 10° | severely decreased |
| -2 | 10 – 14° | moderately decreased |
| 1 | 15 - 20° | assumed normal range |
| +2 | 21 - 25° | moderately increased |
| +3 | > 25° | severely increased |
When we started our investigation we had to introduce a grading system. For the normal range we assumed first, and then tested out that 15 to 20° can be considered the normal range grade 1 for acetabular and femoral anteversion (Tab.2).
| Grade | Range | No. of hips and (%) |
| -3 | < 20 | 110 (38) |
| -2 | 20 - < 30 | 71 (24) |
| 1 | 30 - 40 | 68 (23) |
| +2 | > 40 - 50 | 25 (9) |
| +3 | > 50 | 16 (6) |
At first we tested the correlation between the different angle groups and the range of internal and external rotation and then the absence of pain and osteoarthrosis.
As we learned then, acetabular and femoral anteversion can compensate each other or add to better or negative values. McKibbin, in 1970, has already introduced an instability index by adding up the increased values of acetabular and femoral anteversion together (Tab. 3). At 60 and more, the hip joint became extremely unstable. We took the opposite side and added up the decreased values using the same grades from 1 to -3 and to +3. Our normal range of 15- 20° appears here as 30- 40 if you add it.
This table also shows how frequent decreased anteversion is: Grade -3 in the sum of the index was found in 38%, grade -2 in 24%. This sums up to a total of 62% compared to only 15% of increased anteversion.
The results of long tables I compress in two short sentences. There was a significant correlation between the decreased index -2 and -3 groups and the typical change in range of movement, decreased internal and increased external rotation.
Between the index group -3 and the normal group 1, the confidence interval was also significant for the prevalence of pain and osteoarthrosis at grade -3. In other words: joints with a decreased acetabular and femoral anteversion, both close to zero, have to expect pain and osteoarthrosis, ...
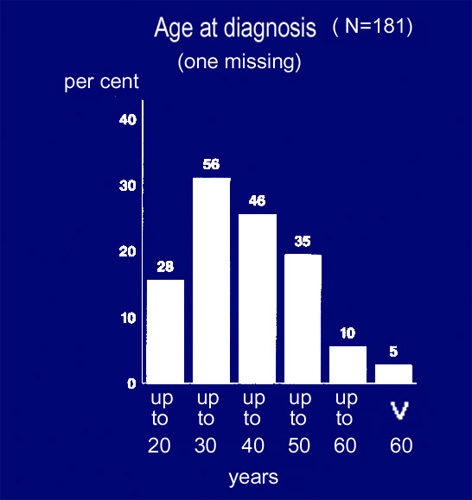 ... most frequently starting between 20 and 30 years already as you see here in the age table of our patients (Fig. 24). Therapy should start then before osteoarthrosis appears.
... most frequently starting between 20 and 30 years already as you see here in the age table of our patients (Fig. 24). Therapy should start then before osteoarthrosis appears.
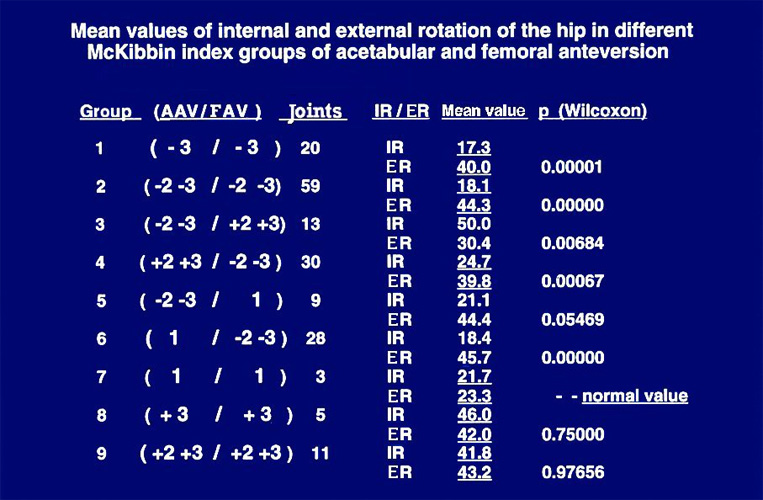 We also tested the possibility of compensation between acetabular and femoral anteversion by compiling 9 different groups with equally increased or decreased or normal values and those where either acetabular or femoral anteversion were minus and the other plus in different degrees or normal (Fig. 25).
We also tested the possibility of compensation between acetabular and femoral anteversion by compiling 9 different groups with equally increased or decreased or normal values and those where either acetabular or femoral anteversion were minus and the other plus in different degrees or normal (Fig. 25).
In these combinations it is striking that the femoral anteversion, whether plus or minus, is the determinative part and the acetabular anteversion is of less influence regarding range of motion, pain and arthrosis. This is important for the indication of femoral rotational osteotomies and triple osteotomies.
 In which patients and deformities do we find decreased values of anteversion?
In which patients and deformities do we find decreased values of anteversion?
First, there is probably a considerable part already present at birth as Pitkow (USA) demonstrated with this graph. After 18-24 months the majority improves and the girls with increased anteversion show up. But especially in males a considerable number of joints with decreased anteversion remains and is larger to my opinion than shown in Fig. 26.
| Slipped capital femoral epiphysis | Grade -2 | Grade -3 | Total |
| Femoral anteversion | |||
| n = 31 hips | 13% | 77% | 90% |
| Acetabular Anteversion | |||
| n = 33 hips | 21% | 27% | 48% |
In patients with a slipped capital femoral epiphysis of a higher degree, but also in patients without complaints and a moderate displacement, anteversion was decreased in 90% at the femor and in 48% at the acetabulum to the degrees -2 and -3 (Tab. 4).
| Coxa vara | Grade -2 | Grade -3 | Total |
| Femoral anteversion | |||
| n = 39 hips | 5% | 77% | 82% |
| Acetabular Anteversion | |||
| n = 39 hips | 23% | 5% | 28% |
In coxa vara the corresponding percentages are 82% for the femor and 28% for the acetabulum (Tab. 5).
| Coxa valga | Grade -2 | Grade -3 | Total |
| Femoral anteversion | |||
| n = 21 hips | 14% | 33% | 47% |
| Acetabular Anteversion | |||
| n = 21 hips | 29% | 29% | 58% |
A smaller percentage is even found in coxa valga where we expect only increased anteversion (Tab. 6).
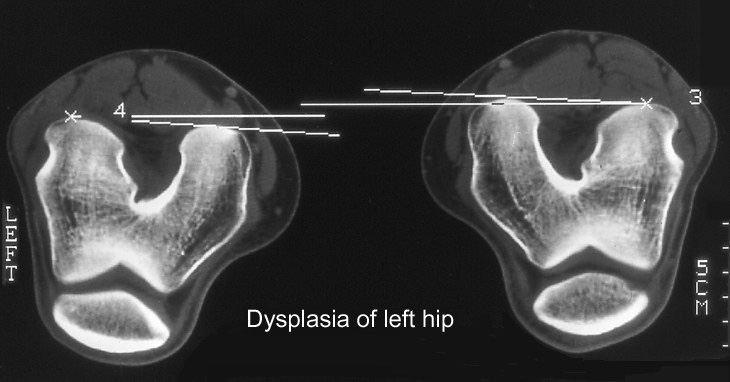
| Dysplasia of the Hip | Grade -2 | Grade -3 | Total |
| Femoral anteversion | |||
| n = 32 hips | 6% | 59% | 65% |
| Acetabular Anteversion | |||
| n = 31 hips | 16% | 29% | 45% |
And also in joints with developmental hip dysplasia, which were investigated separately, femoral anteversion was decreased in 65% and acetabular anteversion in 45%. (Tab. 7) This is important to notice when operations for dysplasia are planned.
| Deep acetabulum | Grade -2 | Grade -3 | Total |
| Femoral anteversion | |||
| n = 36 hips | 14% | 61% | 75% |
| Acetabular Anteversion | |||
| n = 40 hips | 20% | 25% | 45% |
Finally, even in deep acetabula (CE angle of 40-45°), which present the opposite deformity of dysplasia, there are percentages of decreased femoral anteversion of 75% and 45% of acetabular anteversion (Tab. 8).
From these tables I think you can imagine how frequently decreased anteversion can be found in painful hips.
 We also noted decreased anteversion after detorsion-varus-osteotomies in childhood when femoral anteversion was corrected to degree zero and normal anteversion did not develop again, as we see in this 15 year old girl (Fig. 27).
We also noted decreased anteversion after detorsion-varus-osteotomies in childhood when femoral anteversion was corrected to degree zero and normal anteversion did not develop again, as we see in this 15 year old girl (Fig. 27).
We never derotated to zero ourselves, but we have learned, that this has to be counted also among the causes of decreased femoral anteversion.
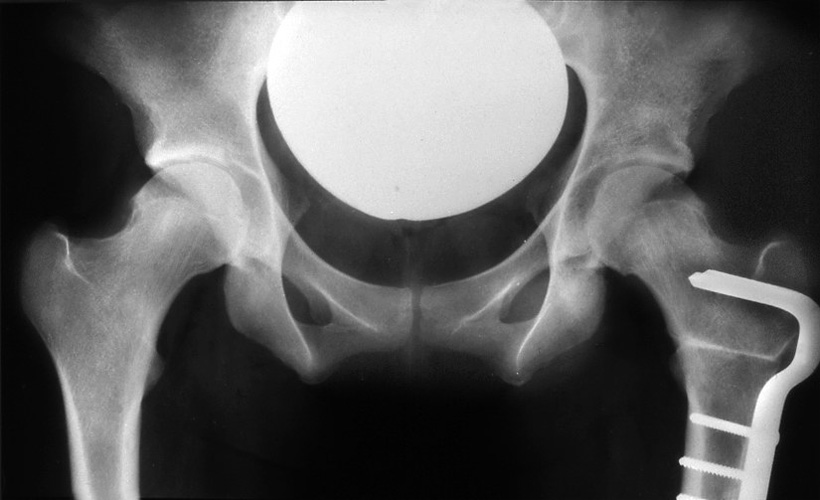
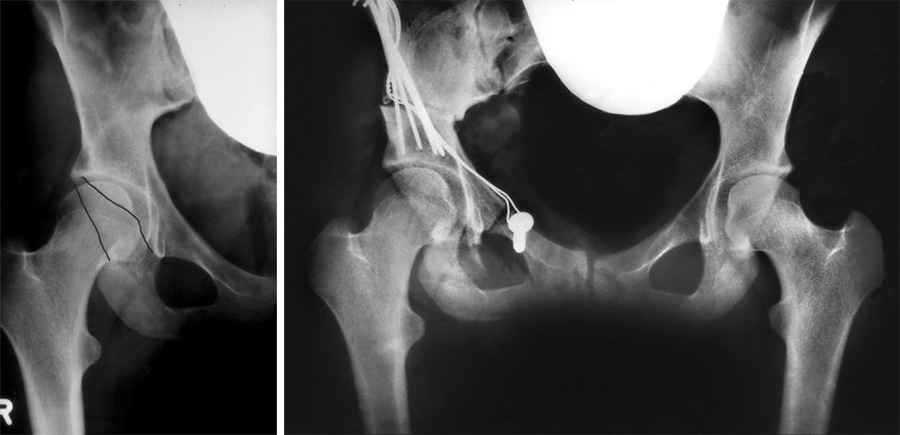
 This 18 year old girl came for triple osteotomy (Fig. 28). Do you note anything else besides of hip dysplasia? The result of triple osteotomy was perfect.
This 18 year old girl came for triple osteotomy (Fig. 28). Do you note anything else besides of hip dysplasia? The result of triple osteotomy was perfect.
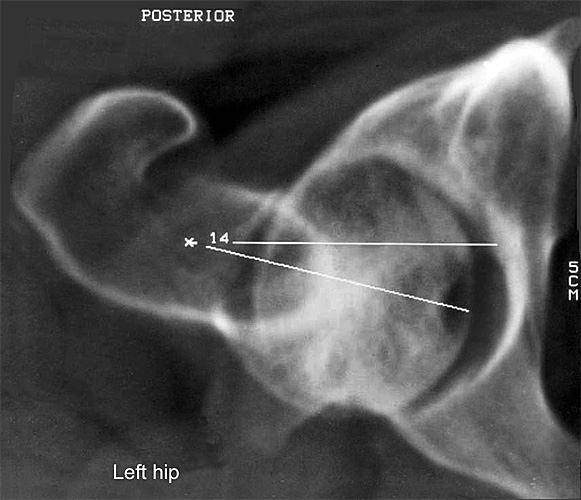
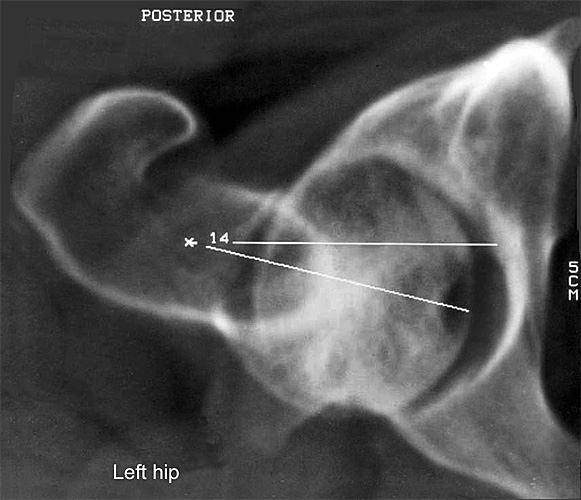
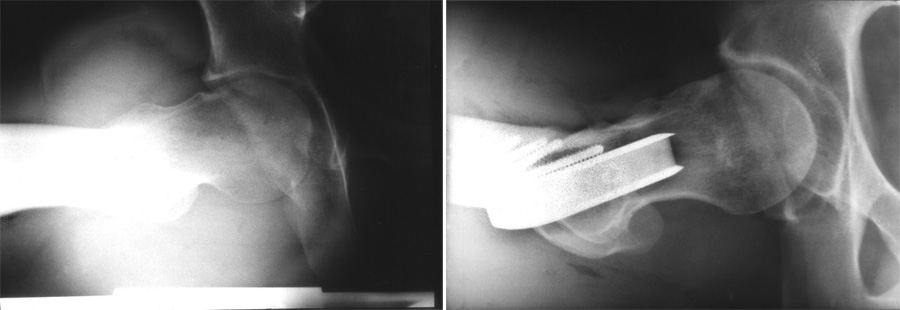
 But 2 1/2 years later she again was admitted because of pain at her hip. We had not realized that her femur, after derotation-varus-osteotomy in childhood, had no anteversion any more (Fig. 29).
But 2 1/2 years later she again was admitted because of pain at her hip. We had not realized that her femur, after derotation-varus-osteotomy in childhood, had no anteversion any more (Fig. 29).
 A rotation osteotomy to the normal femoral anteversion of 15 – 20° was performed and her pain disappeared (Fig. 30). This is the therapy for these patients! We have to normalize the decreased anteversion of the femur or the acetabulum or both in severe cases.
A rotation osteotomy to the normal femoral anteversion of 15 – 20° was performed and her pain disappeared (Fig. 30). This is the therapy for these patients! We have to normalize the decreased anteversion of the femur or the acetabulum or both in severe cases.
 The rotational osteotomy in itself is not difficult. But to equilibrate internal and external rotation, at 45° of flexion, often needs two trials or a third.
The rotational osteotomy in itself is not difficult. But to equilibrate internal and external rotation, at 45° of flexion, often needs two trials or a third.
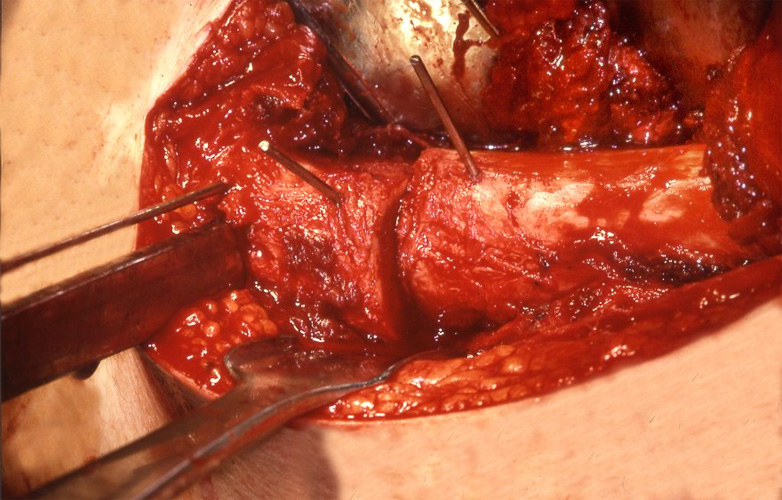
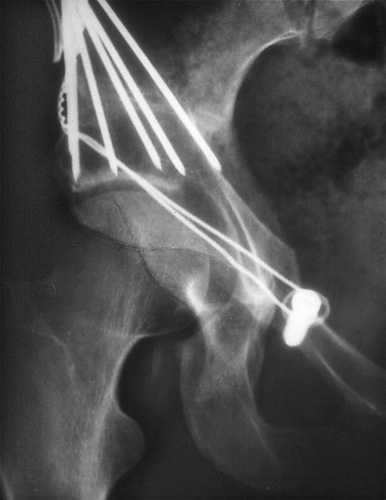
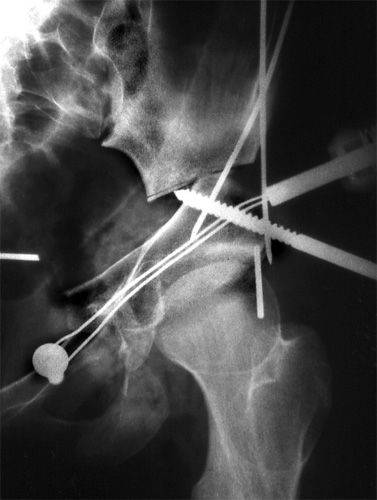
Internal rotation should slightly preponderate. Two Kirschner wires are drilled into the femur towards the central axis, one above and one below the planned osteotomy (Fig. 31). With triangular templates we measure the internal rotation of the distal K-wire.
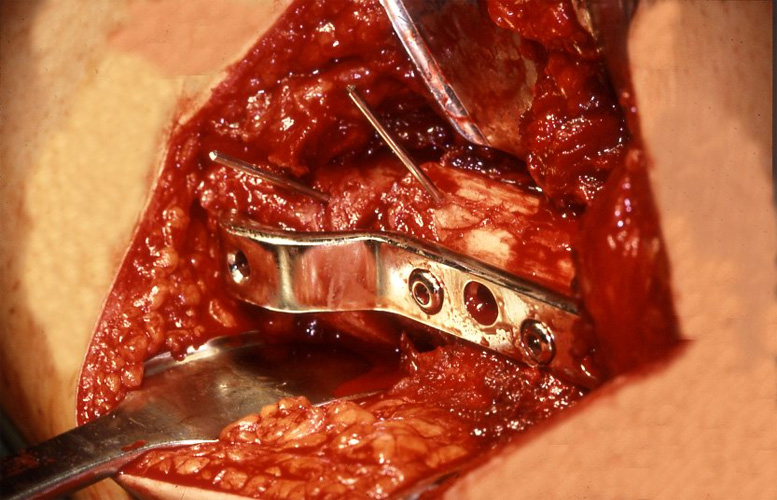 The AO blade plate is fixed first only temporarily with one cortical screw only going fully through and one only half way for testing the internal rotation and increasing the rotation again if necessary (Fig. 32). Internal rotation should be increased to 15 – 20° more than external rotation.
The AO blade plate is fixed first only temporarily with one cortical screw only going fully through and one only half way for testing the internal rotation and increasing the rotation again if necessary (Fig. 32). Internal rotation should be increased to 15 – 20° more than external rotation.
 When we want to figure out the acetabular anteversion in a radiography, the pelvis should not be rotated to the side and not have a tilt, more or less inclination. The normal distance of the anterior and posterior rim of the acetabulum is shown in Fig. 33.
When we want to figure out the acetabular anteversion in a radiography, the pelvis should not be rotated to the side and not have a tilt, more or less inclination. The normal distance of the anterior and posterior rim of the acetabulum is shown in Fig. 33.
 If the anterior rim covers the posterior, an anteversion close to zero must be suspected (Fig. 34).
If the anterior rim covers the posterior, an anteversion close to zero must be suspected (Fig. 34).
 If there is a large distance, anteversion is increased (Fig. 35).
If there is a large distance, anteversion is increased (Fig. 35).
 This is a thing in between. Here anteversion is decreased to a higher degree only in the upper part of the acetabulum (Fig. 36).
This is a thing in between. Here anteversion is decreased to a higher degree only in the upper part of the acetabulum (Fig. 36).
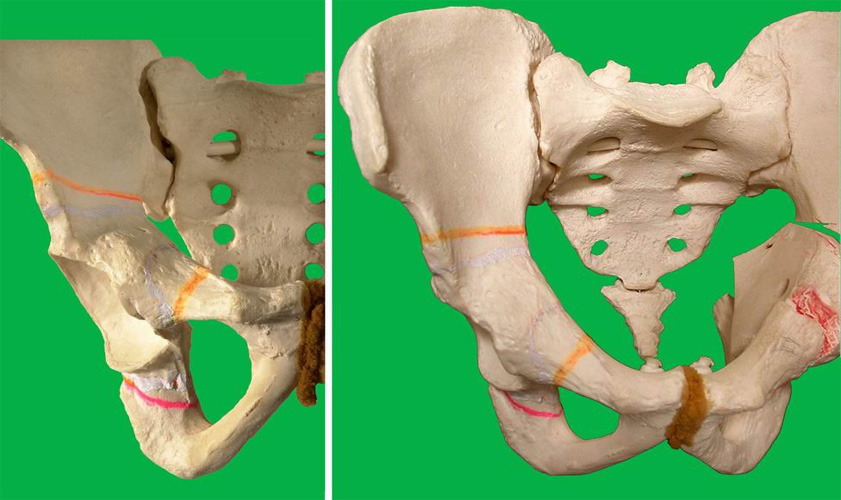
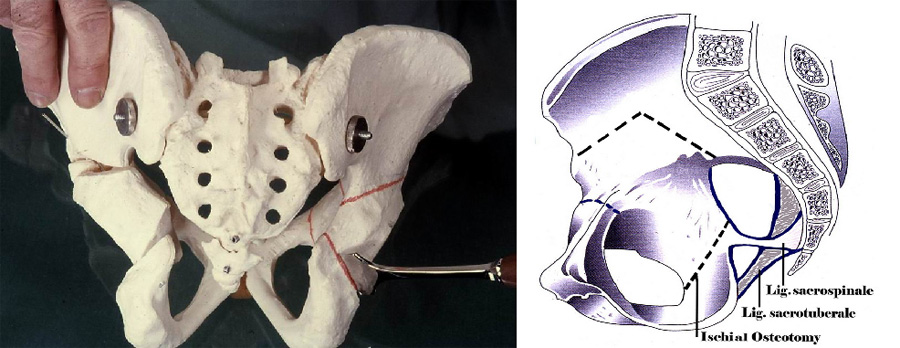 To correct decreased acetabular anteversion we have to rotate the acetabulum internally. This is possible by our triple pelvic osteotomy which releases the acetabular fragment from the two ligaments which connect the ischium with the sacrum. The pubic osteotomy is shown here, too (Fig. 37).
To correct decreased acetabular anteversion we have to rotate the acetabulum internally. This is possible by our triple pelvic osteotomy which releases the acetabular fragment from the two ligaments which connect the ischium with the sacrum. The pubic osteotomy is shown here, too (Fig. 37).
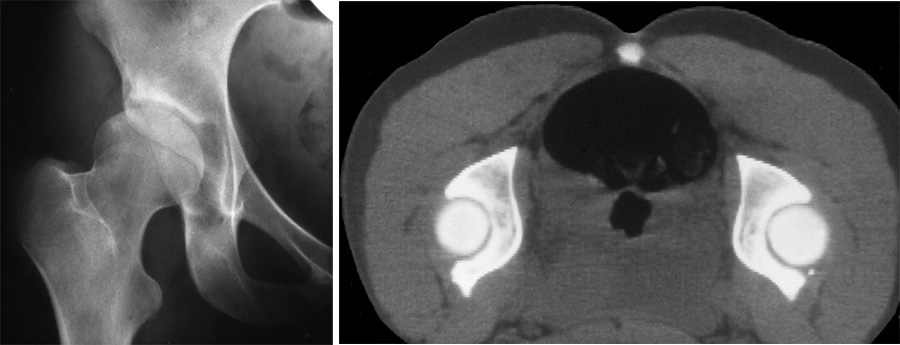 In this hip you see the anterior rim of the acetabulum covering the posterior in the upper part as we saw it already. The tomography confirms it. The hip of this 30 years old woman shows a dysplasia of a medium degree and she felt pain. At 1991 we were not aware of the anteversion problem and performed a normal triple osteotomy (Fig. 38).
In this hip you see the anterior rim of the acetabulum covering the posterior in the upper part as we saw it already. The tomography confirms it. The hip of this 30 years old woman shows a dysplasia of a medium degree and she felt pain. At 1991 we were not aware of the anteversion problem and performed a normal triple osteotomy (Fig. 38).
 The covering was perfect. But the upper rim of the acetabulum appears much deeper now (Fig. 39). A number of surgeons think that they have improved the ventral covering of the femoral head. But this is a mistake.
The covering was perfect. But the upper rim of the acetabulum appears much deeper now (Fig. 39). A number of surgeons think that they have improved the ventral covering of the femoral head. But this is a mistake.
 In this picture the right pelvis is inclined anteriorly and you see how the anteversion differs (Fig. 40). We noted for a long time, that the internal rotation after osteotomy was somewhat decreased. So we rotated it a bit internally until we found the papers of Visser and of Anda.
In this picture the right pelvis is inclined anteriorly and you see how the anteversion differs (Fig. 40). We noted for a long time, that the internal rotation after osteotomy was somewhat decreased. So we rotated it a bit internally until we found the papers of Visser and of Anda.
 They had shown experimentally that with continuous anterior inclination of the pelvis the acetabular anteversion decreases.
They had shown experimentally that with continuous anterior inclination of the pelvis the acetabular anteversion decreases.
Now we postulate: when we rotate the acetabulum first laterally and then anteriorly, we also have to rotate it internally 15 – 20° and check the internal rotation immediately whether it is normal. A small vertical K-wire is helpful to follow the rotation (Fig. 41).
These hips of a 32 years old man have an acetabular anteversion of zero, but a good normal femoral anteversion (Fig. 42 - 43) As we stated already, the femor has more influence on the range of movement and impingement than the acetabulum. This patient complained about pain only occasionally. No operation was performed.
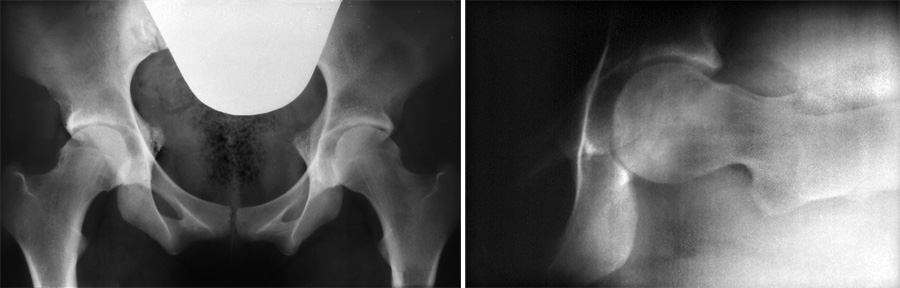
The pelvis of a 20 year old woman presented an extreme deformity of retroverted acetabuli as you see at the obturator foramen and the marked protruding of the ischial spines inside (Fig. 44). The femoral anteversion was also decreased to zero. Her internal rotation was 20°, the external 60°.
 That was in 1983. We performed only a rotational osteotomy of the femur to a normal value (Fig. 45). Two years ago she told me, that she had only moderate pain and that she does not need an additional operation. This is speaking also for the determinative influence of the femoral anteversion.
That was in 1983. We performed only a rotational osteotomy of the femur to a normal value (Fig. 45). Two years ago she told me, that she had only moderate pain and that she does not need an additional operation. This is speaking also for the determinative influence of the femoral anteversion.
However, at an extreme retroversion like this (Fig. 46a, left), we performed an acetabular rotation to improve anteversion (Fig. 46b, right).
Sometimes, when decreased acetabular and femoral anteversion are combined, cysts are found in the acetabular roof and upper parts as shown here,
at an age of 26 years (Fig. 47).

The ap radiography of the left hip is not very striking (Fig. 48).
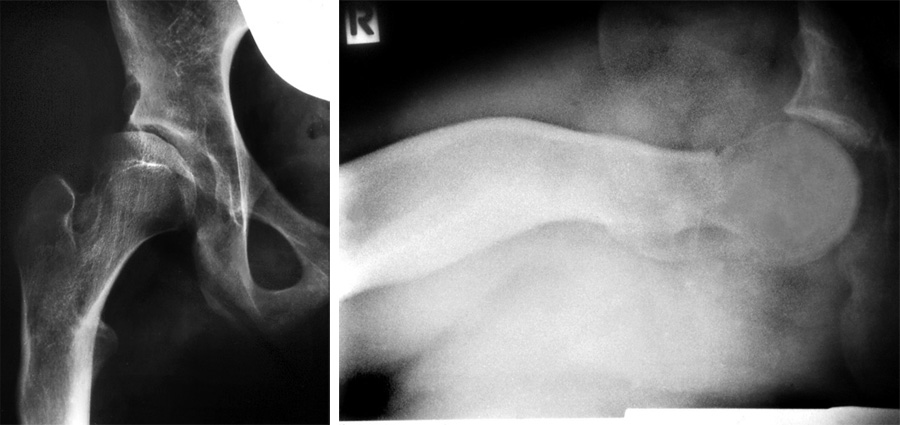
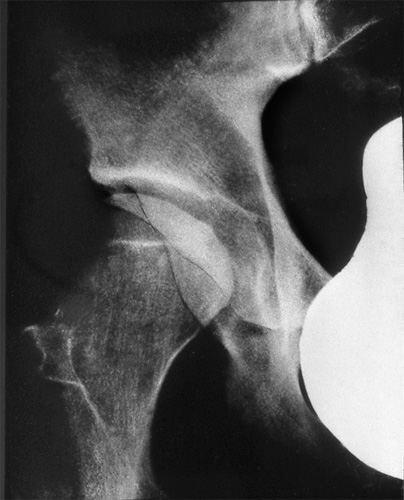
 In slipped capital femoral epiphysis femoral anteversion is nearly always decreased and frequently near zero and may cause by itself the slipping - according to Gelberman - in slight and severe cases (Fig. 49).
In slipped capital femoral epiphysis femoral anteversion is nearly always decreased and frequently near zero and may cause by itself the slipping - according to Gelberman - in slight and severe cases (Fig. 49).
This is also the reason of pain in hips with only moderate slipping. Impingement of the labrum is possible. Anterior rotation osteotomy does improve the complaints. Only in a very severe loss of the femoral neck offset this has to be corrected directly by the technique of Ganz (Fig. 50).
53 years after slipped femoral epiphysis,we find a severe osteoarthrosis of the hip in these tomographies and acetabular and femoral anteversion are zero
(Fig. 51).
Finally we have one report about complaints caused by increased anteversion. This 15 year old girl complained about repeated episodes of a sudden giving-way syndrome of the right knee into flexion and internal rotation when walking. Acetabular anteversion was increased to 27° and femoral anteversion to 23° (Fig. 52). These degrees added, give us an instability index after Mc Kibbin of 50°. This explains the complaints.
 A triple osteotomy with external rotation of the acetabulum of about 15° took away her complaints. The preoperative radiography shows a large distance of the two acetabular rims. Postoperatively this distance is normal.
A triple osteotomy with external rotation of the acetabulum of about 15° took away her complaints. The preoperative radiography shows a large distance of the two acetabular rims. Postoperatively this distance is normal.
If you want a take-home-message, then it is this: When internal rotation of the hip at 45° of flexion is decreased and the external rotation is increased, order x-ray and CT for diagnosis of decreased acetabular and femoral anteversion. This causes of osteoarthrosis and impingement and slipped femoral epiphysis is too often overlooked.
| Download | |
|---|---|
| Decreased acetabular and femoral Anteversion, a Cause of Impingement, slipped femoral epiphysis and Osteoarthritis of the Hip | PDF (15.2MB) |