Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Developmental hip disorders - Acetabular Dysplasia
© Prof. Dr. med. Dietrich Tönnis
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
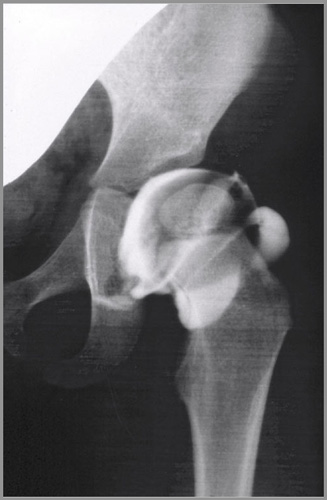
 In acetabular dysplasia the acetabulum is not spherical, it is oval. The upper margin may be deficient not only laterally, as seen here, but also anteriorly and posteriorly (Fig. 1).
In acetabular dysplasia the acetabulum is not spherical, it is oval. The upper margin may be deficient not only laterally, as seen here, but also anteriorly and posteriorly (Fig. 1).
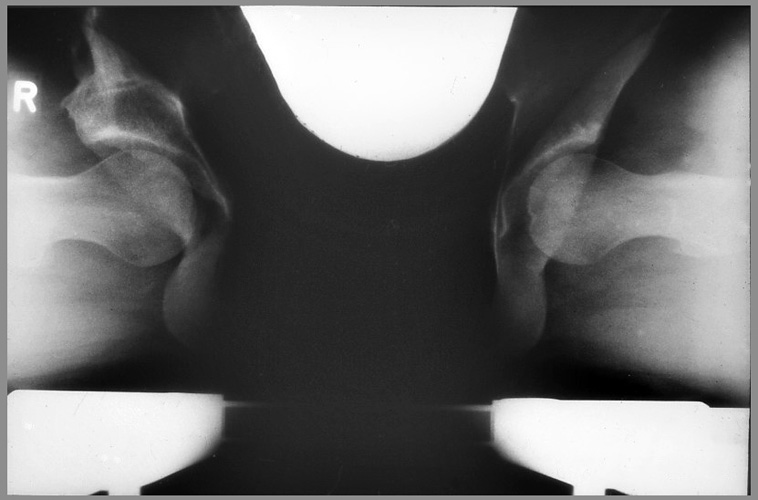
 This is the lateral view of the dysplastic acetabulum after Lequesne and deSeze (Fig. 2). The VCA angle measures the anterior coverage and should be not less than 25° in adolescents and adults.
This is the lateral view of the dysplastic acetabulum after Lequesne and deSeze (Fig. 2). The VCA angle measures the anterior coverage and should be not less than 25° in adolescents and adults.
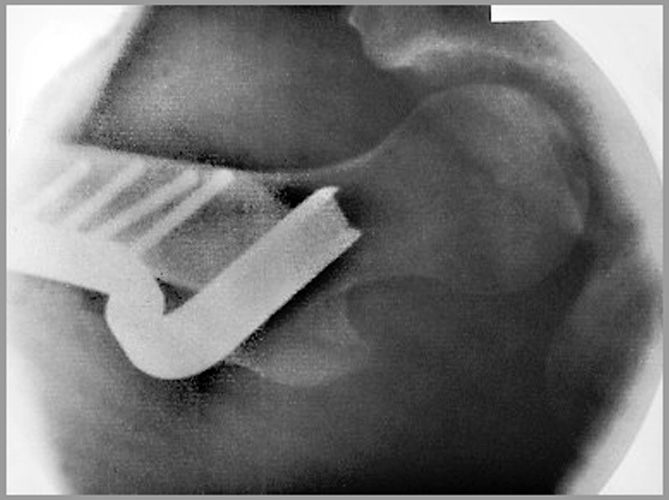
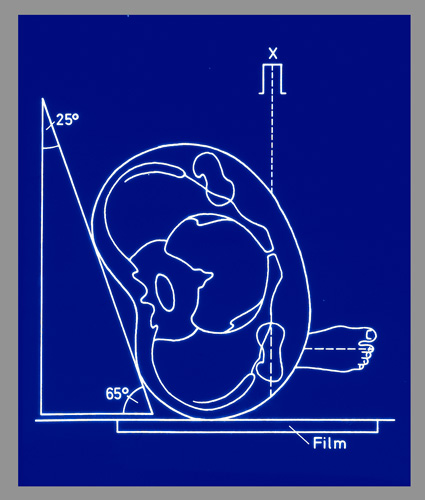 The patient is turned back 25° with the opposite side of the pelvis. Then a single picture of the other hip is possible (Fig. 5).
The patient is turned back 25° with the opposite side of the pelvis. Then a single picture of the other hip is possible (Fig. 5).
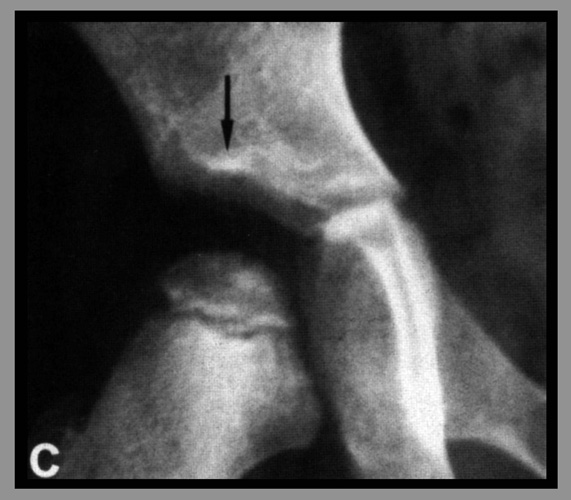 The lateral acetabular rim is sometimes seen separately in x-rays, where the sourcil ends more medial than the anterolateral portion of the acetabulum (Fig. 6). Ogata et al. and Kim et al. have demonstrated the details.
The lateral acetabular rim is sometimes seen separately in x-rays, where the sourcil ends more medial than the anterolateral portion of the acetabulum (Fig. 6). Ogata et al. and Kim et al. have demonstrated the details.
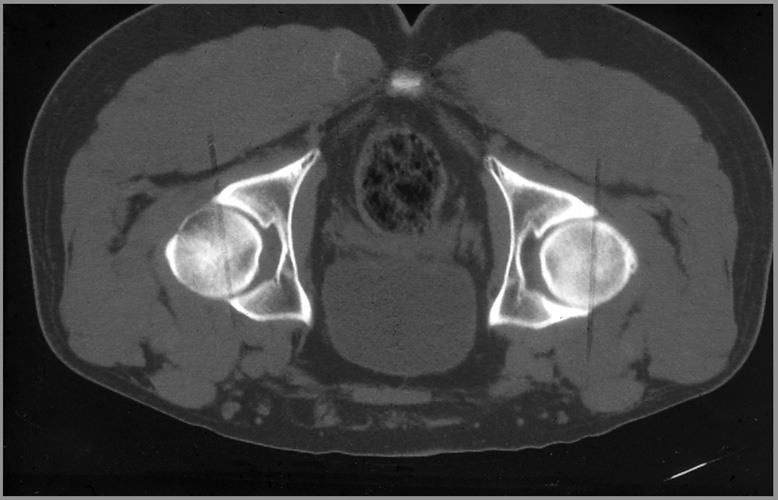
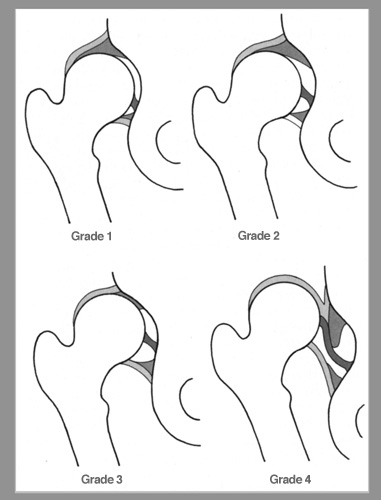
 Grade 1 here, the acetabular roof in the CT is normally shaped as a broad rhomb. In grade 4, the severe dysplasia, it has more the form of a banana. In the a.p. radiography, however, the picture can change with lateral rotation of the pelvis or with decreased anteversion of the acetabulum (Fig. 7).
Grade 1 here, the acetabular roof in the CT is normally shaped as a broad rhomb. In grade 4, the severe dysplasia, it has more the form of a banana. In the a.p. radiography, however, the picture can change with lateral rotation of the pelvis or with decreased anteversion of the acetabulum (Fig. 7).
Congenital acetabular dysplasia is mainly caused by external factors of the uterus, lack of space and amniotic fluid, also breech positions, especially with extended knees. Therefore it is called developmental. The legs are pressed against the body of the child and the femoral head against the lateral and posterior acetabular rim. By the time the cartilagineus and the bony rim are deformed and the capsule and the labrum are distended.
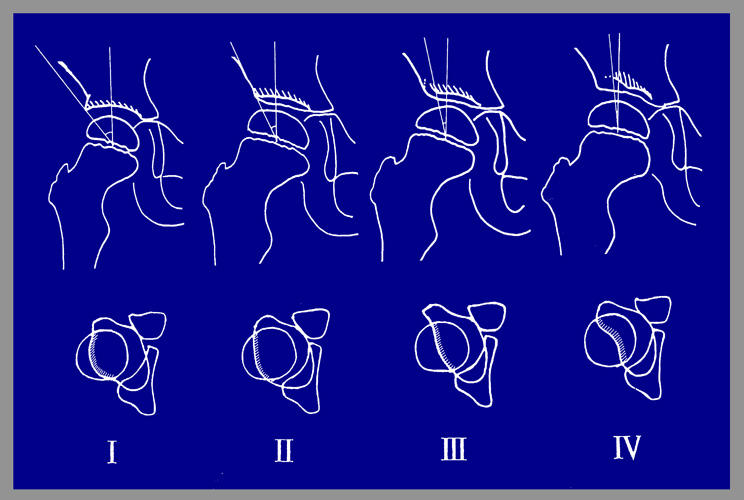
 Then instability is found in palpatory examination, either inside the joint, or, when the femoral head can be pushed up to the acetabular rim and snaps back with Ortolanis click (Fig. 8). The next degrees are marked by the fully dislocatable femoral head and the dislocated, but not reducible femoral head.
Then instability is found in palpatory examination, either inside the joint, or, when the femoral head can be pushed up to the acetabular rim and snaps back with Ortolanis click (Fig. 8). The next degrees are marked by the fully dislocatable femoral head and the dislocated, but not reducible femoral head.
| 1 | Mildly unstable hip without snapping sign |
| 2 | Subluxatable hip with Ortolanis snap of entry |
| 3 | Dislocatable and reducible hip |
| 4 | Fully dislocated, irreducible hip |
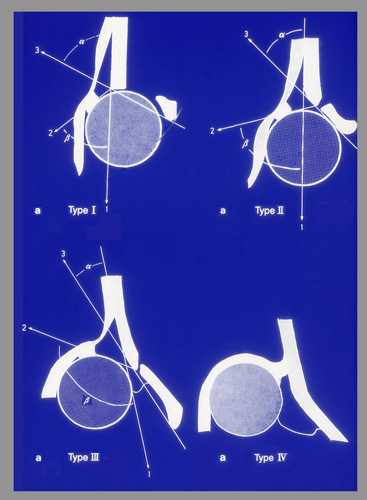
Howarth and Dunn have also described these different grades anatomically. In Grafs type 3 and Howarth`s grade 1 the femoral head has left the acetabulum, but the labrum is still on its top (Fig. 10).
In the full dislocation the femoral head ascends higher and pushes the labrum back and deforms the cartilaginous rim to a protruding roll. This is a high, usually not reducible dislocation (Fig. 11, 12). The newborn screening has to verify whether the femoral head is reducible without resistance. Then abduction pillows, splints or in dislocations of grade 3 plaster casts in "human position" can be applied until stability is achieved. In this child the femoral head is standing in the reduction position at the actabular entrance.
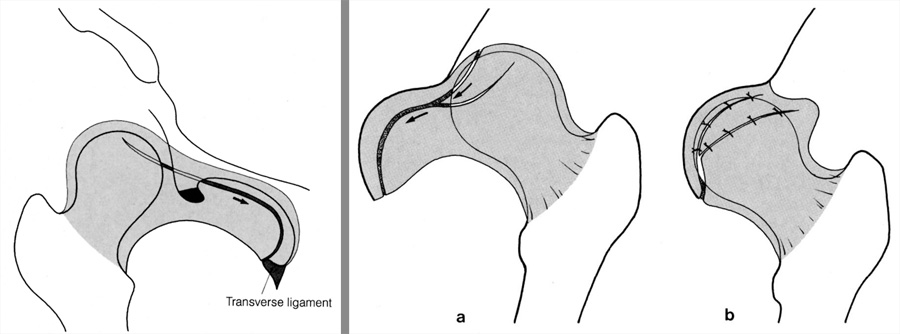
But between the bulging big upper labrum and the protruding transverse ligament , the femoral head cannot pass into the joint (Fig. 12).
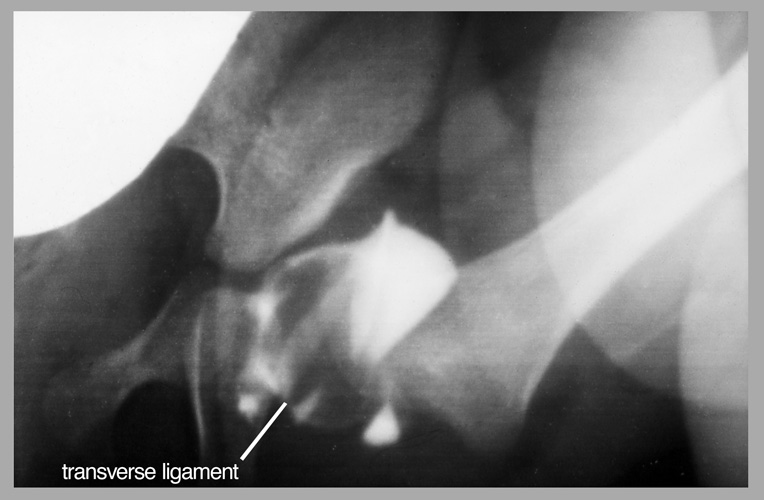 This is a sufficient reduction. The femoral head is placed here beneath the upper labrum. The transverse ligament is seen somewhat protruding too. But the femoral head has reached the bottom of the acetabulum (Fig. 13).
This is a sufficient reduction. The femoral head is placed here beneath the upper labrum. The transverse ligament is seen somewhat protruding too. But the femoral head has reached the bottom of the acetabulum (Fig. 13).
 If a deep reduction of the femoral head is not possible, we try traction in longitudinal direction for 3-4 weeks (Fig. 14).
If a deep reduction of the femoral head is not possible, we try traction in longitudinal direction for 3-4 weeks (Fig. 14).

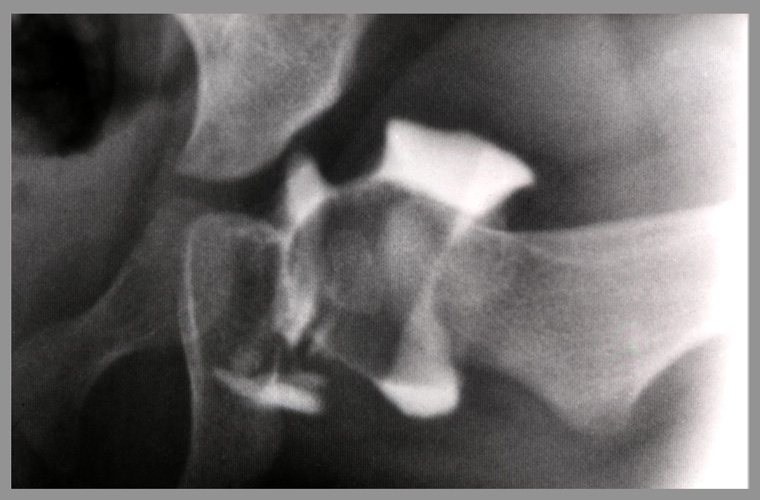
A reduction against a narrow acetabular inlet causes avascular necroses, the more, the severe the constriction is, and if there is no femoral ossific nucleus as here, or a very retarded, it is a high risk (Fig. 15).

You see the necrosis at the right (Fig. 16). In younger children we can wait, also if traction is not sucessive. Open reduction is performed then in the second half year.
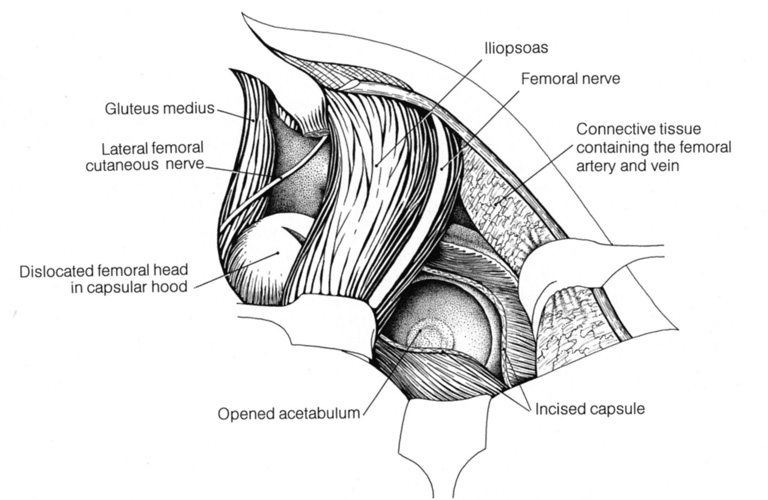
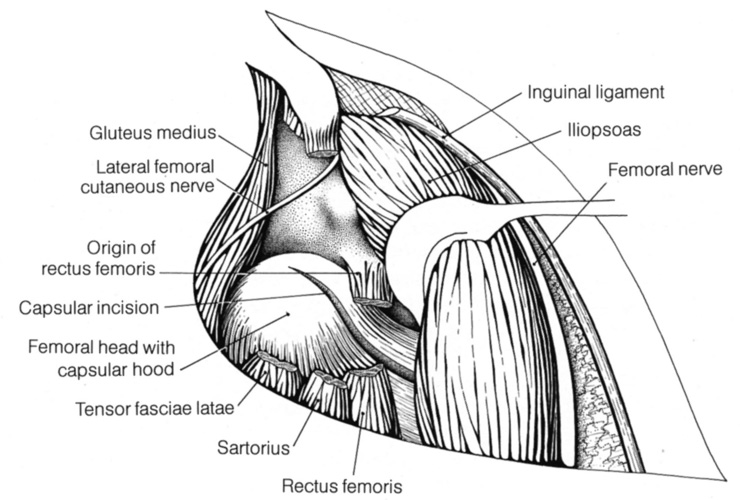
... then medial of the psoas muscle. Inside the lacuna musculorum we approach the joint and retract the lacuna vasorum carefully medially without opening (Fig. 18).
This offers a good visibility of the medial part of the joint, where the transverse ligament has to be dissected without trauma to the acetabular artery and vein in the acetabular fossa.
A capsulorraphy is added, and in the second year of life, if there is still dysplasia, in addition an acetabuloplasty with transiliac osteotomy (Fig. 19).
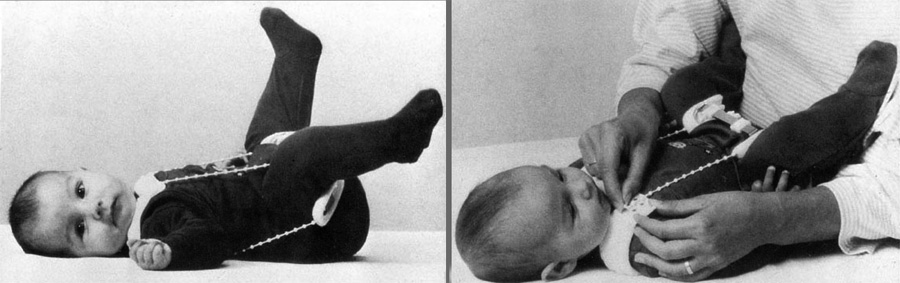
The main principle in conservative and operative treatment is to achieve a deep reduction and a good stability of the joint. In moderate dysplasias, in the first half year, flexion-abduction pillows and splints are sufficient.
Fig. 20 shows the Tübinger splint of Bernau which we prefer. The Pavlik harness has no fixed and moderate abduction, takes longer time and may redislocate.
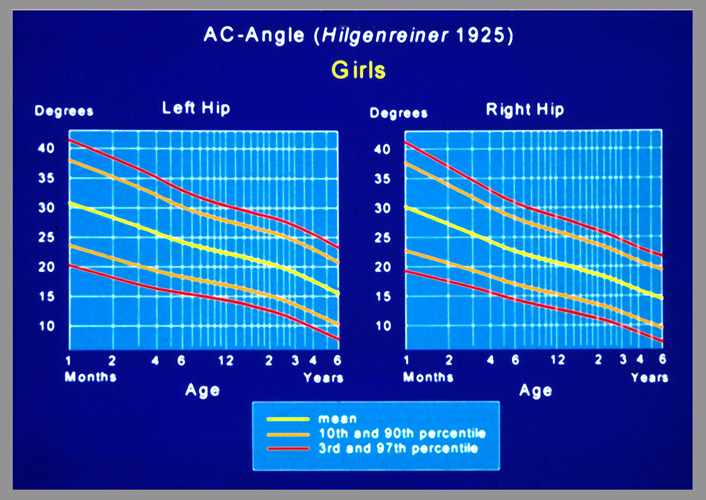
If the acetabular index is not normalized at the age of 6 months in our percentilgraph of Neidel, a plaster cast in the second half year must be applied (Fig. 21). Also in closed reductions of dislocations it is optimal to give a cast in human position with 110-120° of flexion and between 45 and 60° of abduction as it seems necessary for stability. When changing the plaster cast every 4-6 weeks, stability is palpated and then a splint can be applied, also, if radiography shows progress of acetabular roof improvement.
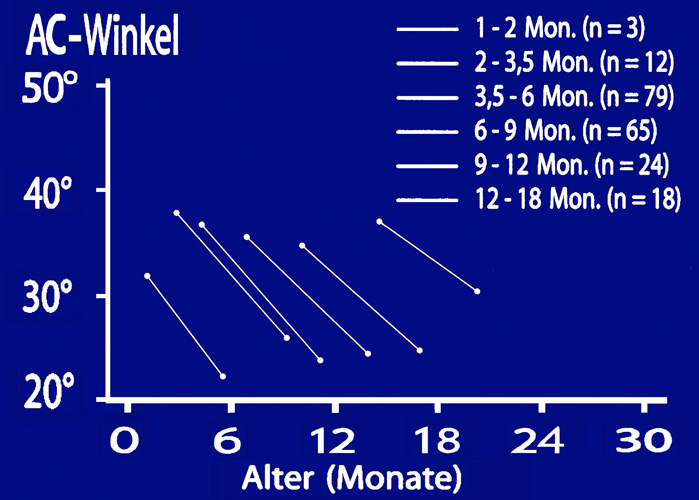
Even in older children up to 1 1/2 years a longer treatment with plaster casts can still normalize the acetabular index (Fig. 22).

The most effective operative improvement of the dysplastic acetabular roof can be achieved with what Dega called the transiliac osteotomy. Actually Wiberg in 1953 and Chapchal in 1965 have published it already (Fig. 23).
 We used it also after this time and osteotomized the ilium fully up to the sciatic notch posteriorly and medially almost up to the posterior triradiate cartilage. The actabular roof is levered down then close to the triradiate cartilage zone.
We used it also after this time and osteotomized the ilium fully up to the sciatic notch posteriorly and medially almost up to the posterior triradiate cartilage. The actabular roof is levered down then close to the triradiate cartilage zone.
Today we use bone wedges prepared from femoral heads of the bone bank to keep the acetabulum in the normal position.
This operation is possible until 9-10 years and sometimes later and achieves a very good correction up to 50 degrees (Fig. 25 and 26). Simultaneous varus osteotomies are usually not necessary and result frequently in a head-to-neck position with a shortening of the femoral neck. We have not used it any longer.
In adolescents and adults, the dysplastic acetabulum has to be fully mobilized by osteotomizing the connections to the pubis, the ischium and the ilium. Then a free rotation in all 3 planes can normalize the coverage of the femoral head. Le Ceur and Hopf started with it in 1965 and 66 and others with different modifications later.
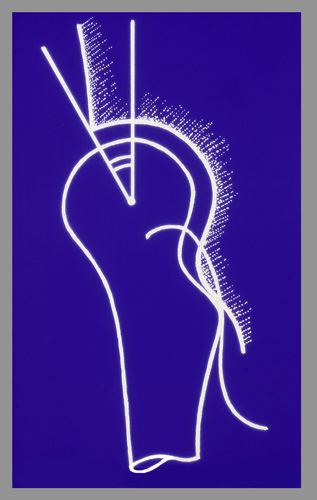
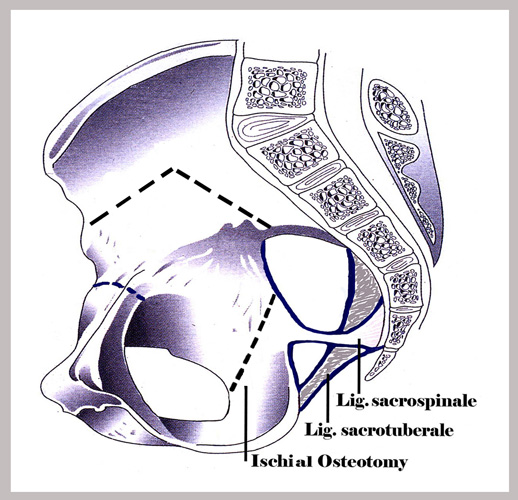 Today our modification of 1977 and following that of Ganz 1984 have the highest numbers of operations and good results. The ischium is osteotomized from a dorsal gluteal approach. The osteotomy runs from the sciatic notch to the obturator foramen and has to be directed anteriorly not less than 10° and not much more than 30° (Fig. 27). The rotation of the acetabulum is not hindered then by the sacroischial ligaments, and these are left in the normal place for bony consolidation later. The ilium osteotomy is interrupted by an anterior angle to minimize a ventral gap after anterior rotation.
Today our modification of 1977 and following that of Ganz 1984 have the highest numbers of operations and good results. The ischium is osteotomized from a dorsal gluteal approach. The osteotomy runs from the sciatic notch to the obturator foramen and has to be directed anteriorly not less than 10° and not much more than 30° (Fig. 27). The rotation of the acetabulum is not hindered then by the sacroischial ligaments, and these are left in the normal place for bony consolidation later. The ilium osteotomy is interrupted by an anterior angle to minimize a ventral gap after anterior rotation.
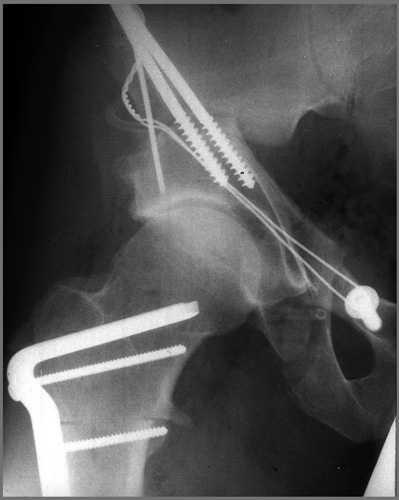
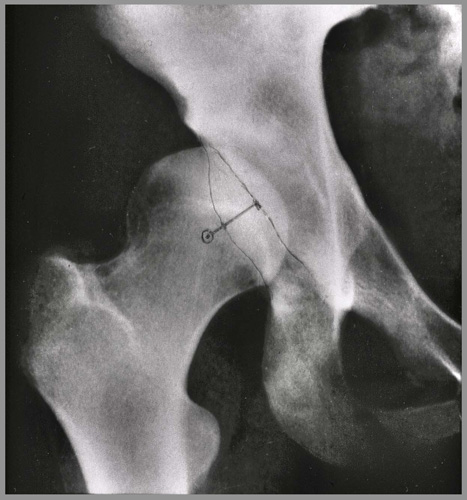
 After the pubic osteotomy we shift the lateral part of the pubis not only higher, but also medially to medialize the joint for biomechanical reasons (Fig. 28).
After the pubic osteotomy we shift the lateral part of the pubis not only higher, but also medially to medialize the joint for biomechanical reasons (Fig. 28).
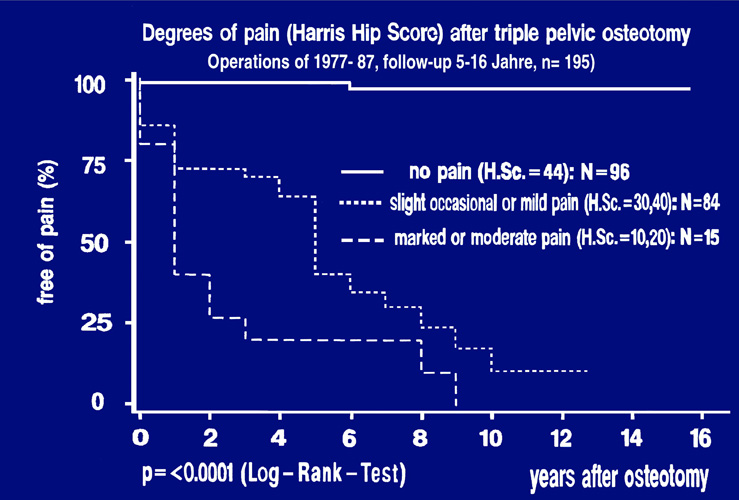 The results after 5-16 years in 195 joints I can show you briefly in this survingrate curve regarding pain. Included were all degrees of decentration of a joint from the spherical to the higher dislocated and the false joints (Fig. 29).
The results after 5-16 years in 195 joints I can show you briefly in this survingrate curve regarding pain. Included were all degrees of decentration of a joint from the spherical to the higher dislocated and the false joints (Fig. 29).
That is the reason that only 49,2%, so practically 50%, are fully free of pain. They are represented in the upper horizontal curve. 43% had or developed occasional or slight pain as we see in the moderatly descending curve, and 7,7% had a marked or moderate pain.

Beside the congenital developmental acetabular dysplasia there is a later developing dysplasia during growth where there is a functional coxa valga. Here the originally normal acetabular margin stands under a higher pressure of the decentered femoral head for instance at the opposite side of a shorter leg or at the opposite side of a joint stiff in abduction (Fig. 30).

Also an extreme coxa valga antetorta can deform the anterolateral rim of the joint in the course of time. Very important to know is the fact, that in childhood and adolescence pain is felt usually very late when deformation is already extreme. This is different from the adults. Therefore controlls are more necessary in children and adolencents (Fig. 31).
 So far we have discussed only acetabular deformities of two planes. The third one, the horizontal plane, is shown by the computer tomography: the anteversion of the acetabulum and femoral neck
So far we have discussed only acetabular deformities of two planes. The third one, the horizontal plane, is shown by the computer tomography: the anteversion of the acetabulum and femoral neck
(Fig. 32).
So far the interest of the orthopedic surgeons was directed mainly to the increased femoral anteversion. But the joints with decreased femoral anteversion are much more frequent and cause more pain and osteoarthrosis.
 In the a.p. pelvic radiography we can only suppose from the full appearance of the length of the femoral neck that there is little or no anteversion (Fig. 33)
In the a.p. pelvic radiography we can only suppose from the full appearance of the length of the femoral neck that there is little or no anteversion (Fig. 33)
 And in the acetabulum the distance of the anterior and posterior acetabular rim should be 1-1,5 cm measured on a vertical line from the center of the femoral head (Fig. 34). But with lateral rotations of the pelvis and different degrees of pelvic inclination, the picture is changed.
And in the acetabulum the distance of the anterior and posterior acetabular rim should be 1-1,5 cm measured on a vertical line from the center of the femoral head (Fig. 34). But with lateral rotations of the pelvis and different degrees of pelvic inclination, the picture is changed.
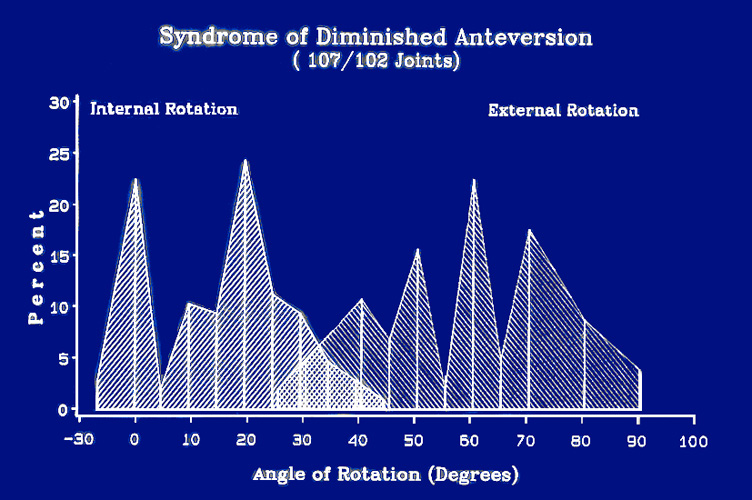 Suspicion of decreased anteversion of the femur and perhaps in addition the acetabulum is given when the internal rotation of the hip is decreased and the external increased to about the double value.
Suspicion of decreased anteversion of the femur and perhaps in addition the acetabulum is given when the internal rotation of the hip is decreased and the external increased to about the double value.
In this figure you see the very low values of internal rotation and towards the right the high range of external rotation in these patients (Fig. 35).
This deformity is found already after birth. Anomalies of gait may be seen early in extreme cases and first pain is felt at about 10 years (Fig. 36 - 38).
We found severely decreased femoral anteversion in 77% percent in the slipped capital femoral epiphysis, even when it was asymptomatic and only a pistol grip deformity; also regularly in coxa vara and frequently in hip dysplasia too. Statistical investigations in 356 hips with tomographies proved a correlation between the added angles and the range of movement, pain and osteoarthrosis.
The therapy consists in rotation osteotomies of the femur to a normal anteversion of 15-20° (Fig. 39 and 40).
When acetabular anteversion is missing or retroversion is present, a rotation of the acetabulum by triple pelvic osteotomy can be performed (Fig. 41 and 42). Details were published in the American Journal of Bone and Joint Surgery 1999.
We have to conclude: in the acetabulum a number of deformities can be found after birth and later. Early investigation and consequent treatment to achieve stability and normal measurements are successful. Operative procedures are also developed to a high standard with good results.
| Download | |
|---|---|
| Developmental hip disorders - Acetabular Dysplasia | PDF (8.8MB) |