Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Diagnosis and Treatment of Developmental Hip Dysplasia – Our Experience
© Prof. Dr. med. Dietrich Tönnis
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
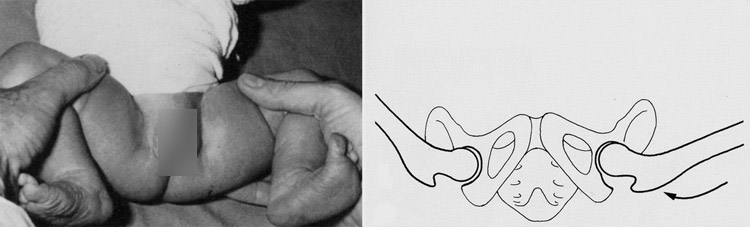
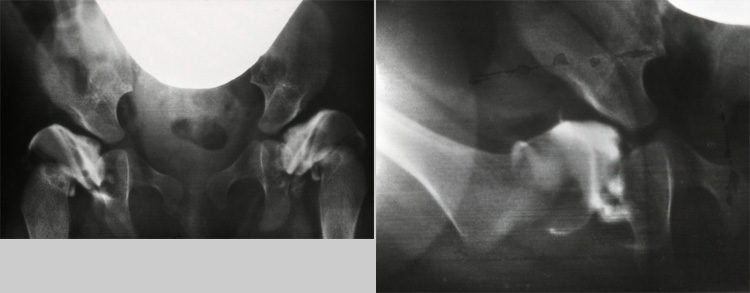
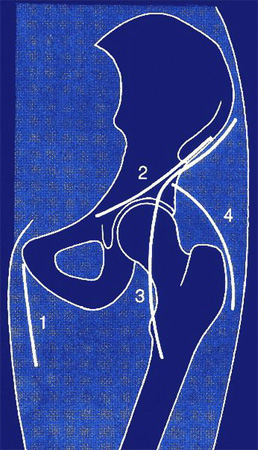
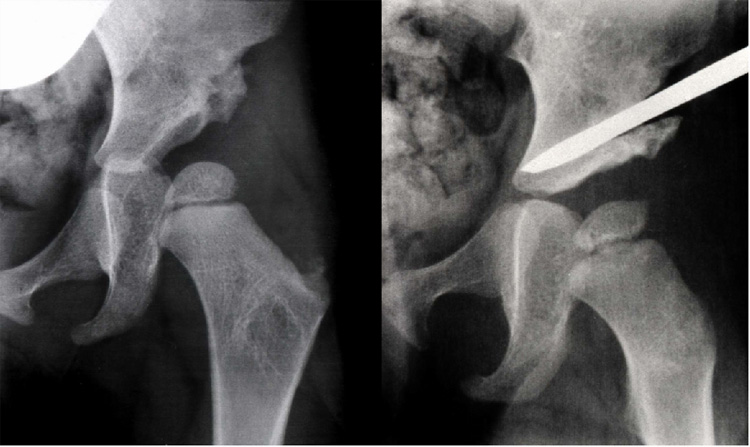
 Hip dysplasia, most frequently, develops during the last months of pregnancy by breech position, lack of amniotic fluid and narrowness in the uterus for different reasons. With extreme flexion, external or internal rotation, the femoral head is pressed against the acetabular margin. Thus the capsule of the joint is distended and the acetabular rim flattened, as we see it here.
Hip dysplasia, most frequently, develops during the last months of pregnancy by breech position, lack of amniotic fluid and narrowness in the uterus for different reasons. With extreme flexion, external or internal rotation, the femoral head is pressed against the acetabular margin. Thus the capsule of the joint is distended and the acetabular rim flattened, as we see it here.
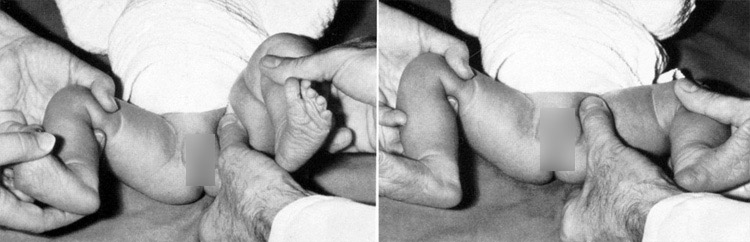
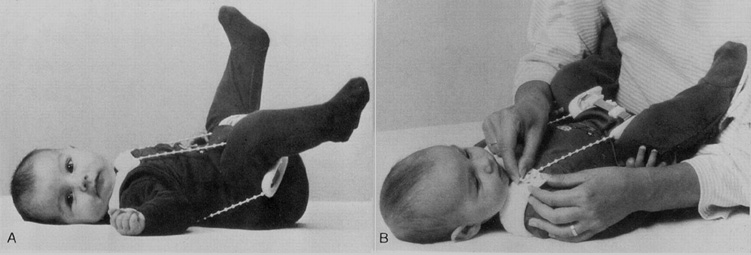
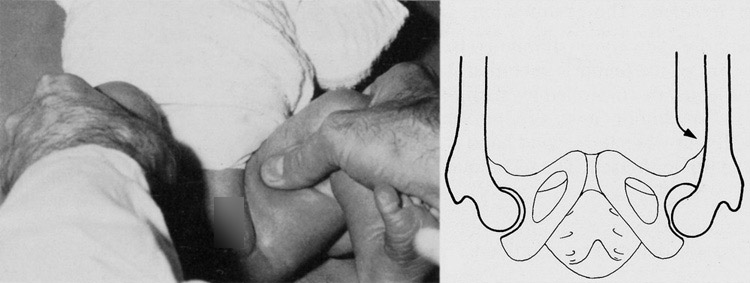 In a marked dysplasia the characteristic sign is instability of the hip. In the provocation test of Coleman and Barlow the 90° flexed and adducted hip is pressed laterally with the thumb, to find out, how far the femoral head is dislocatable.
In a marked dysplasia the characteristic sign is instability of the hip. In the provocation test of Coleman and Barlow the 90° flexed and adducted hip is pressed laterally with the thumb, to find out, how far the femoral head is dislocatable.
We classify in degrees : first the mildly unstable hip, where the femoral head is dislocatable only inside the flattened joint, then the subluxatable head up to the rim and fully reducible with slight snapping on abduction. Next the dislocated hip, outside the joint, but not passing the labrum, mostly reducible. Finally the type luxated beyond the labrum, where reduction is not possible or incomplete. Before 1983 we performed only this examination in our obstetric department and asked for risk factors.
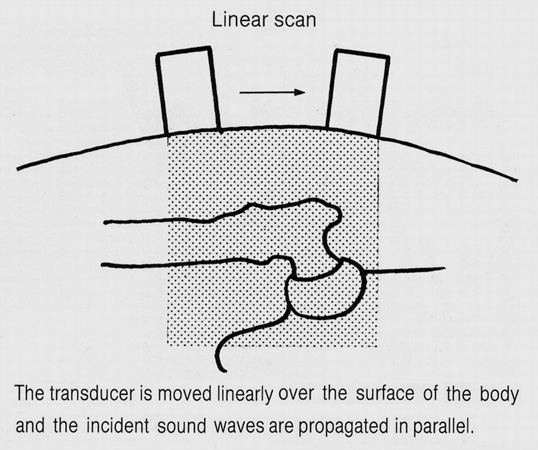 In 1983 we introduced the ultrasound or sonographic examination according to Graf with a linear scan and are still performing it in all newborns. In addition all children get a free follow-up examination after 4 to 6 weeks either by a pediatric or orthopeadic colleague, which is financed by the government.
In 1983 we introduced the ultrasound or sonographic examination according to Graf with a linear scan and are still performing it in all newborns. In addition all children get a free follow-up examination after 4 to 6 weeks either by a pediatric or orthopeadic colleague, which is financed by the government.
 We image the hip joint on a frontal plane of section. Therefore the orientation is similar to an AP radiograph. Structures composed of hyaline cartilage appear devoid of echoes on sonograms. The intermuscular septa, being composed of collagen fibers, are more strongly echogenic than the intervening muscles. The best echo of course comes from the surface of bones.
We image the hip joint on a frontal plane of section. Therefore the orientation is similar to an AP radiograph. Structures composed of hyaline cartilage appear devoid of echoes on sonograms. The intermuscular septa, being composed of collagen fibers, are more strongly echogenic than the intervening muscles. The best echo of course comes from the surface of bones.
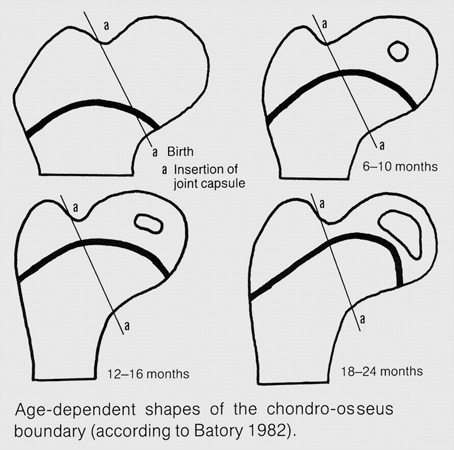 In the newborn and the first months there is a changing chondro-osseus boundery. The greater trochanter, the lateral femoral neck and the femoral head are cartilagenous and the femoral neck in total is not yet developed.
In the newborn and the first months there is a changing chondro-osseus boundery. The greater trochanter, the lateral femoral neck and the femoral head are cartilagenous and the femoral neck in total is not yet developed.
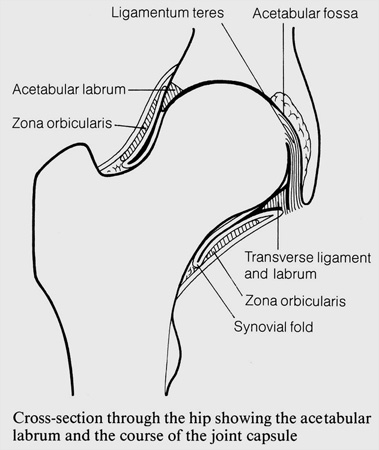 An important structure is the acetabular labrum which surrounds the femoral head at the acetabular rim. Medially it is fused with the transverse ligament. The joint capsule is surrounded by ligaments and the zona orbicularis.
An important structure is the acetabular labrum which surrounds the femoral head at the acetabular rim. Medially it is fused with the transverse ligament. The joint capsule is surrounded by ligaments and the zona orbicularis.
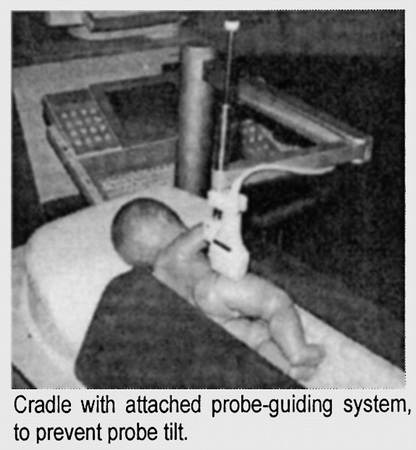
 To obtain a correct sonogram in the frontal plane, the section should go through the midportion of the acetabular roof, not anteriorly or posteriorly and not cranially or caudally.
To obtain a correct sonogram in the frontal plane, the section should go through the midportion of the acetabular roof, not anteriorly or posteriorly and not cranially or caudally.
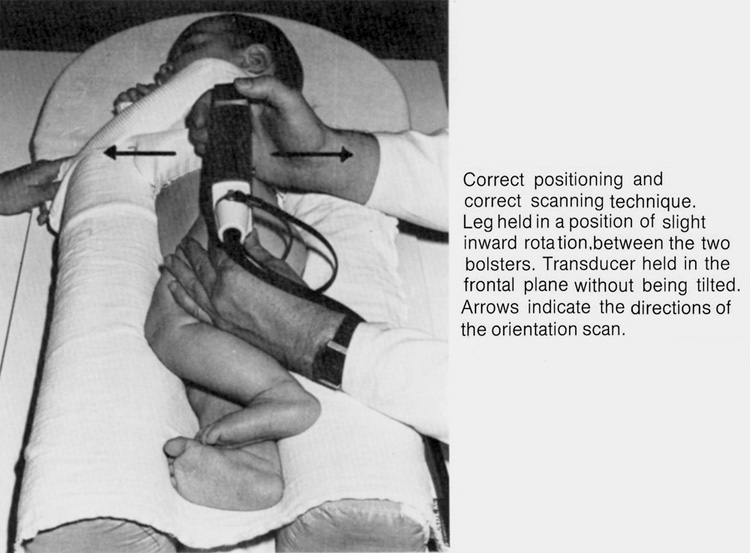 The child is lying in a positioning device of two softly padded bolsters, which are molded for the body.
The child is lying in a positioning device of two softly padded bolsters, which are molded for the body.
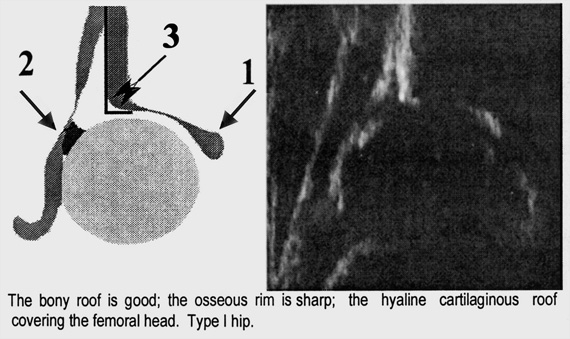
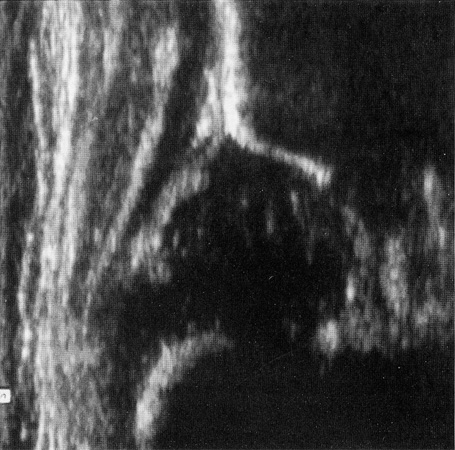
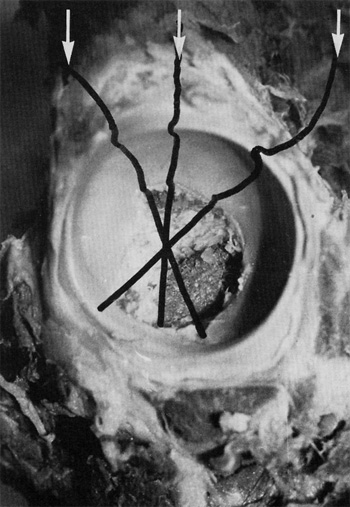
To define a plane in 3 D, three landmarks are absolutely necessary. Otherwise you cannot use the picture. No. 1 is the lower limb of the os ilium, No. 2 the acetabular labrum and No. 3 is the middle section of the bony acetabular roof as we have seen it before from lateral, shown this time here with the ilium in a straight vertical surface.
The osseus acetabular rim can be sharp or blunt. Behind it, there is a so called acoustic shadow, if the acetabular angle is high.
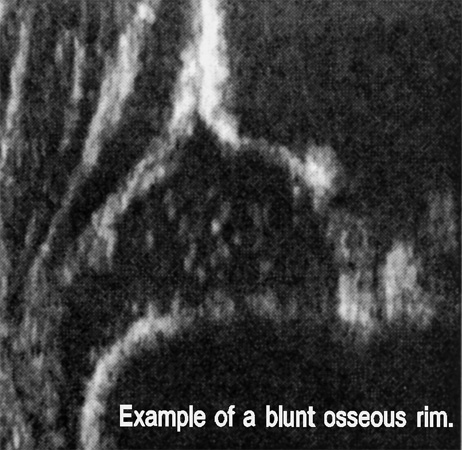 In this sonogramm the acetabular rim is blunt. That is to be seen in the hip type 2. As a fourth landmark the chondro-osseus borderline of the femur should always be visible to the same extent as shown here.
In this sonogramm the acetabular rim is blunt. That is to be seen in the hip type 2. As a fourth landmark the chondro-osseus borderline of the femur should always be visible to the same extent as shown here.
 For the measuring of acetabular angles the bony rim of the acetabulum is defined as the most lateral point of the concavity of the bony socket. At this point the acetabular roof changes to the convexity of the ilium.
For the measuring of acetabular angles the bony rim of the acetabulum is defined as the most lateral point of the concavity of the bony socket. At this point the acetabular roof changes to the convexity of the ilium.
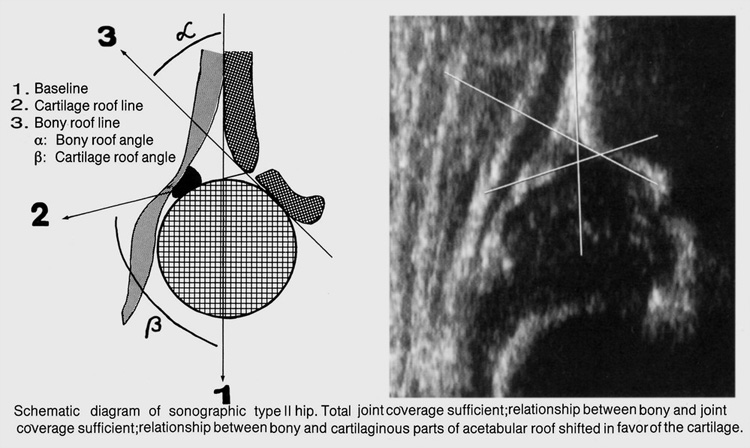
In this picture No. 1 is the base line for both angles. Line 2 starts from the acetabular rim and runs down to the labrum. Here we have a cartilagineus coverage. Thererfore the beta angle is the cartilage angle. No. 3, the alpha angle, is the bony roof angle. At the right you find the angles in a sonogram, alpha 57°, beta 75° in a 6 week old child.
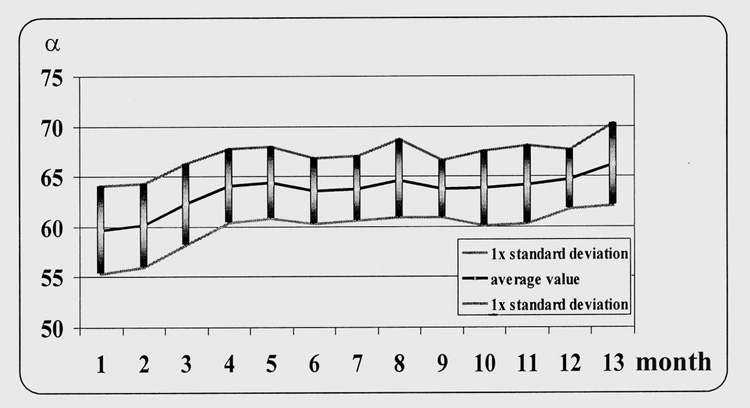
Graf and Tschauner have published a maturation curve of normal joints and so-called physiologically immature joints.
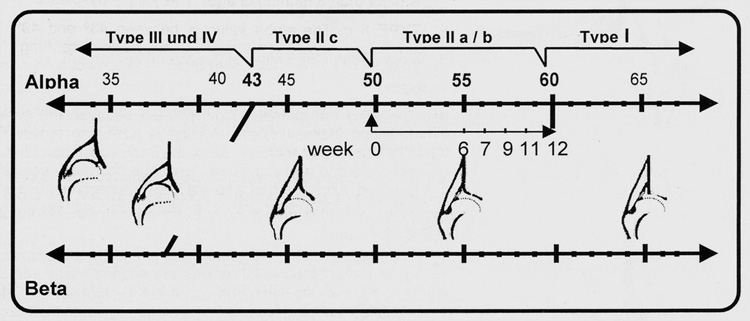
This table Graf calls a sonometer. Let us look at the alpha values which are placed along the upper line. Type 1 has the normal angle and 65 ° should be reached after 12 weeks. Type 2 a with an angle between 50 and 59° is called a physiologically immature joint. Within 12 weeks it should show 60 degrees and more. Broad diapering or a Frejka pillow are useful. After 3 months, if there are still only 50 to 60°, they are characteristic for a dysplastic joint 2 b. In the type 2c the alpha angle lies between 43 and 49°.
This hip socket is severely dysplastic and is close to decentering. 2 c hips can be seen at any age.
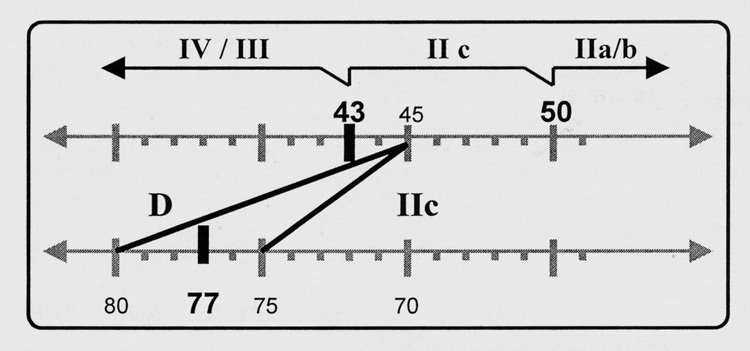
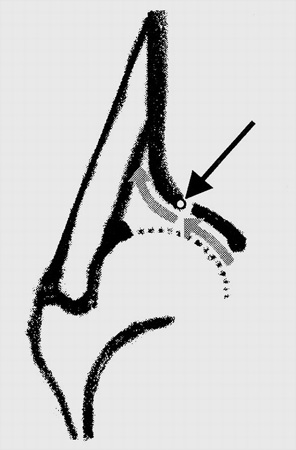
In type 2c joints, where the bony coverage is very poor, decentering can occur. The cartilaginous acetabular roof bends cranially, the beta angle increases, whereas the alpha angle of the bony roof stays the same. This type Graf calls d, or "about to decenter". The beta angle is then in the range of 75° to 80°.

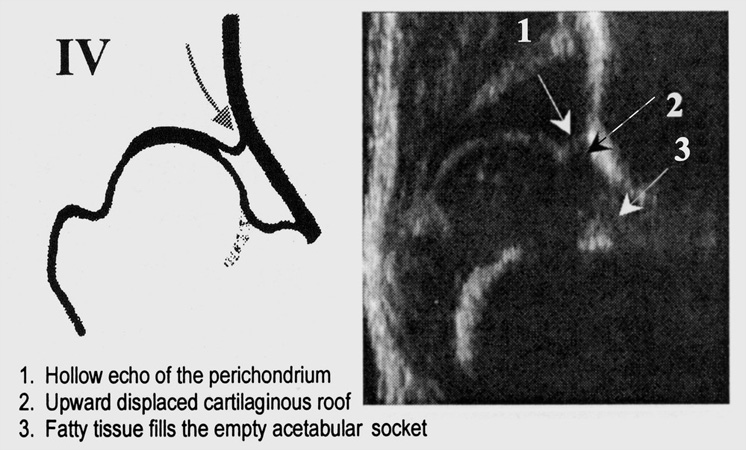
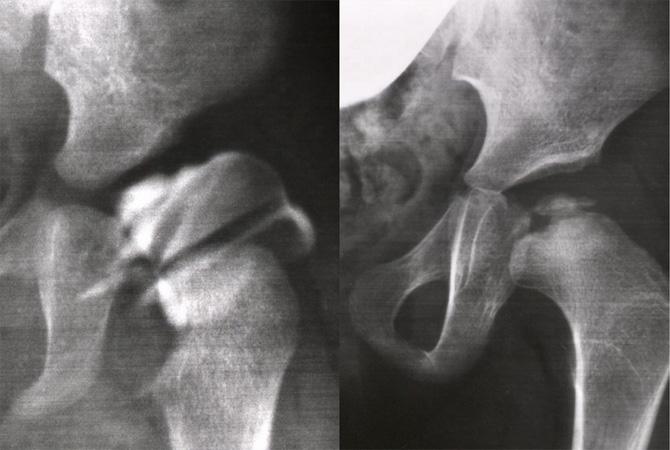
Here we can compare sonography and radiography. Beta angle 76°, so just a type d of Graf. Alpha angle 53°. In the x-ray the ossific femoral nucleus is still very small. In the sonogram the femur is somewhat adducted and the ossific nucleus may therefore be a little more lateral in this 8 week old infant about to decenter.
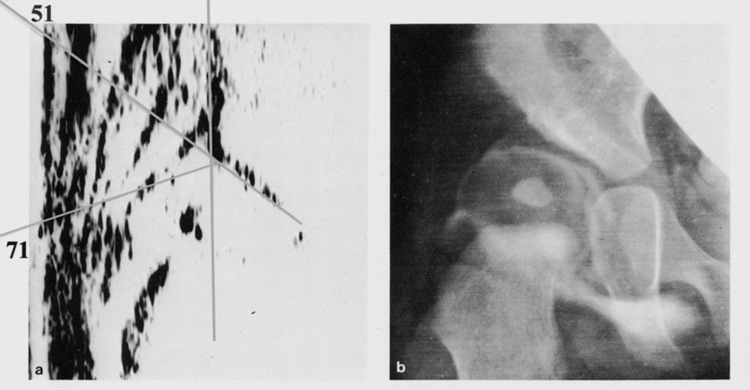
Another comparism: In this 6 month old child the beta angle is 71°, close to the 75° - borderline of the type d. We have to call it a 2c type close to d. In the arthrography the bony acetabular rim has almost disappeared, but the cartilage rim and labrum are still seen on top of the femur. The femur has decentered already to some degree. Type 2c is a severe dysplasia and this child is on the borderline to type d. The sonogram and radiography in these pictures present the same information.
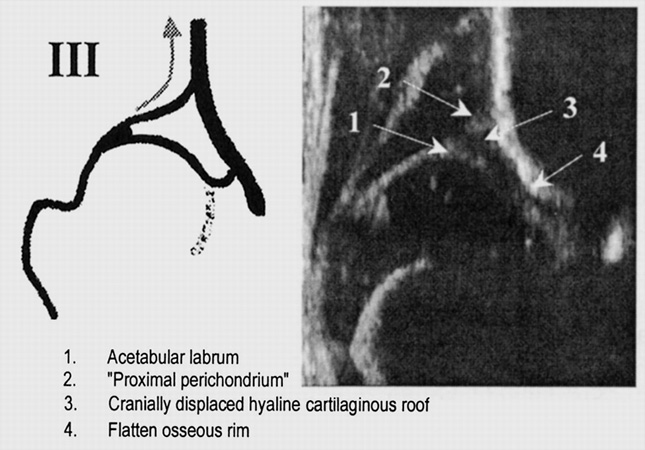
Type 3 and 4 after Graf are the dislocated or decentered types. In type 3 the femoral head takes the cartilaginous acetabular roof and labrum along, when it moves higher. The way to the acetabulum frequently, but not always, remains open.
In type 4 the femoral head glides higher up over the cartilaginous roof and labrum and pushes them back to the acetabulum, usually blocking the entrance together with an elongated transverse ligament.
This is a comparison of a type 3 hip in sonogram and arthrography. The child was 3 month old. The bony rim of the acetabulum is in both pictures flattened and runs continuously with the ilium above. The cartilage rim has also been flattened. The tip of the labrum terminates in a little pool directly above the ossific nucleus and shows an identical location on the sonogram.
The results of our sonographic newborn screening were investigated by Storch on more than 5000 hips. He found 2.64% pathological joints from type 2c to 4. When he added the physiologically immature joints, which became dysplastic at longer controlls, the percentage raised up to to 6.5% pathological joints. Grill, in a collective statistics of Austria, found also 6.57%.
However, the palpatory investigations of the newborns were positive in 100% only in type 4 hips. Typ 3 in 18.5% was not palpated and diagnosed, type d not in 57% and 2c not in 66%. This demonstrates that the dysplasias of type 2 and type d and even some type 3 hips were found only by sonography. That is no overdiagnosis. For colleagues who are interested I want to mention that Graf presents courses every year in summer in England.
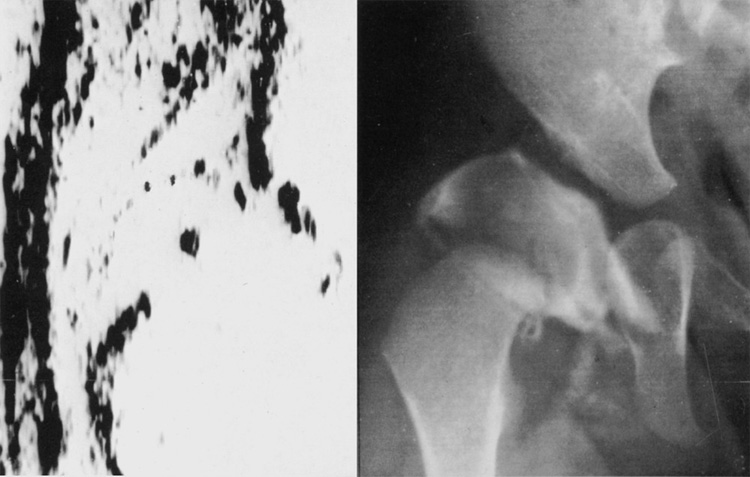
 The treatment of the newborn immature hip and the dysplasias of type 2 and d , we begin with a soft bandage, and 4 weeks later with this fixed flexion-abduction socalled Tübinger splint.
The treatment of the newborn immature hip and the dysplasias of type 2 and d , we begin with a soft bandage, and 4 weeks later with this fixed flexion-abduction socalled Tübinger splint.
We do not use the Pavlik-harness any more. The healing is safer and proceeds faster when there is continuous abduction and flexion.
 In the types 3 and 4 a plaster cast in the squatting position after Fettweis or human position after Salter obtains the best results.
In the types 3 and 4 a plaster cast in the squatting position after Fettweis or human position after Salter obtains the best results.
 However, it must be provided, that the acetabular inlet is not as narrowed, as in this arthrogram, between the protruding lower labrum plus ligamentum transversum on the lower side, and on the upper side a bulging and deformed cartilagineous acetabular lateral rim.
However, it must be provided, that the acetabular inlet is not as narrowed, as in this arthrogram, between the protruding lower labrum plus ligamentum transversum on the lower side, and on the upper side a bulging and deformed cartilagineous acetabular lateral rim.
 When the ossific femoral nucleus is not present and the cartilageneous femoral head has to mold its way against resistance, avascular necrosis develops as we can see here at the right.
When the ossific femoral nucleus is not present and the cartilageneous femoral head has to mold its way against resistance, avascular necrosis develops as we can see here at the right.
Now for the statistics: when the ossific nucleus was developed, the rate of avascular necrosis was only 0.9%. When it was missing or retarded in appearance, the percentage raised from 4.4 to 12.5%.
| Development ossific necleus | Necrosis (%) | Joints (no.) |
|---|---|---|
| normal | 0.9 | 109 |
| missing | 4.5 | 110 |
| small | 8.7 | 85 |
| retarded | 12.5 | 16 |
In addition, the rate of necrosis rised even up to 25% the more lateral the femoral head was standing in the flexion-abduction position for reduction. Then, apparently the resistance for the soft femoral head was too high and the blood circulation was critically decreased.
| Distance (mm) | Necrosis (%) | Joints (no.) |
|---|---|---|
| 0 - 2 | 2.7 | 150 |
| 3 - 5 | 4.1 | 123 |
| 6 - 11 | 25.0 | 16 |
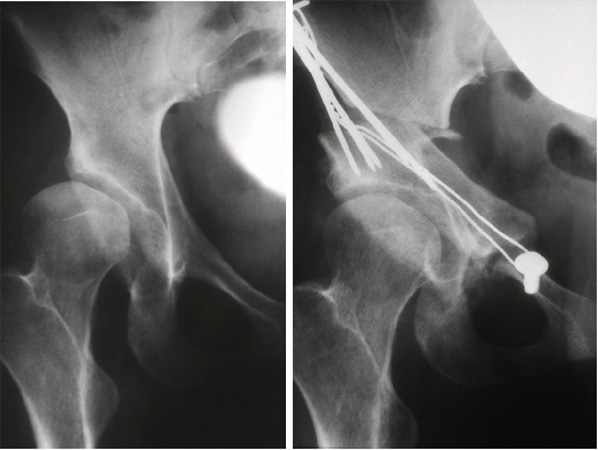
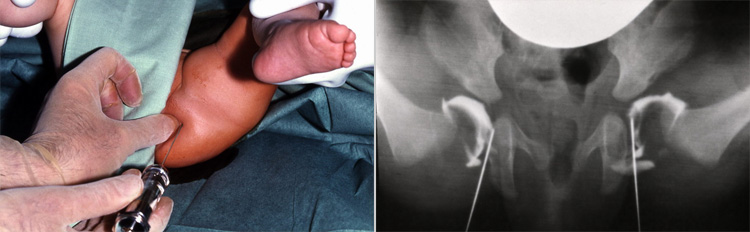 If the femoral head is manually not reducible, arthrography is indicated in the flexion-abduction position. We perform it from distally, and medially of the femoral head. The thumb is placed on the ischial tuberosity. Under control of the image intensifier the needle is inserted next to the thumb and pushed upwards to the acetabular roof and then slightly retracted.
If the femoral head is manually not reducible, arthrography is indicated in the flexion-abduction position. We perform it from distally, and medially of the femoral head. The thumb is placed on the ischial tuberosity. Under control of the image intensifier the needle is inserted next to the thumb and pushed upwards to the acetabular roof and then slightly retracted.
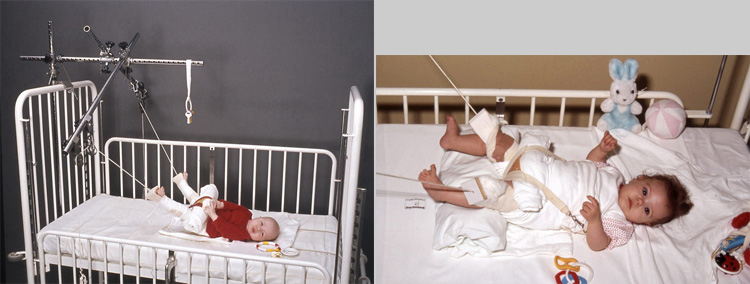 In case the femoral head is not deeply reducible, longitudinal traction of the legs is indicated in slight flexion and abduction. Then the lower labrum plus transverse ligament, which were drawn upwards with the dislocation, are placed below the acetabular inlet, and this way often, the femoral head can enter. If reduction is not possible after 2 to 3 weeks, open reduction is indicated. The ossific femoral nucleus is not of importance in our open reduction.
In case the femoral head is not deeply reducible, longitudinal traction of the legs is indicated in slight flexion and abduction. Then the lower labrum plus transverse ligament, which were drawn upwards with the dislocation, are placed below the acetabular inlet, and this way often, the femoral head can enter. If reduction is not possible after 2 to 3 weeks, open reduction is indicated. The ossific femoral nucleus is not of importance in our open reduction.
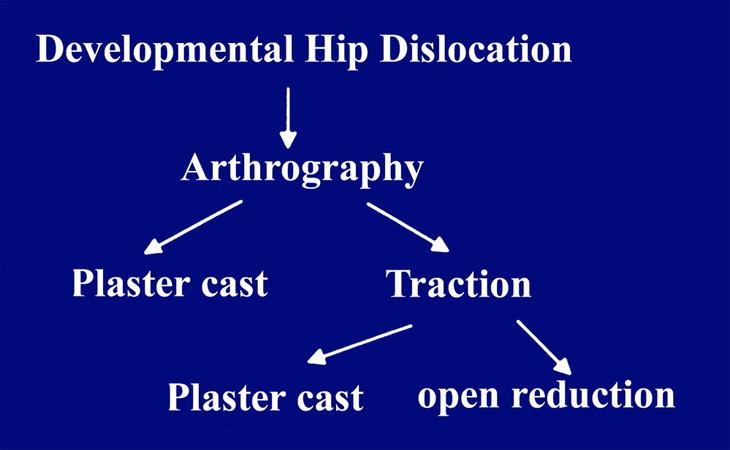 Traction, however, is not possible in the newborns. In this case, we send them home without any orthosis. 2 months later reduction often succeeded. This is our scheme of handling. It is the way to avoid avascular necrosis to the greatest extent.
Traction, however, is not possible in the newborns. In this case, we send them home without any orthosis. 2 months later reduction often succeeded. This is our scheme of handling. It is the way to avoid avascular necrosis to the greatest extent.
 Arthrography shows you more in detail than sonography whether the acetabular inlet is open or not. Here we can see that in a type 3b hip of Graf the elongated Lig. capitis and upper labrum and the protruding lower labrum plus transverse ligament are blocking the reduction.
Arthrography shows you more in detail than sonography whether the acetabular inlet is open or not. Here we can see that in a type 3b hip of Graf the elongated Lig. capitis and upper labrum and the protruding lower labrum plus transverse ligament are blocking the reduction.
 Type 3 b without ossific nucleus has the highest rate of necrosis with 12.5%, while type 4 only had only 5%.
Type 3 b without ossific nucleus has the highest rate of necrosis with 12.5%, while type 4 only had only 5%.
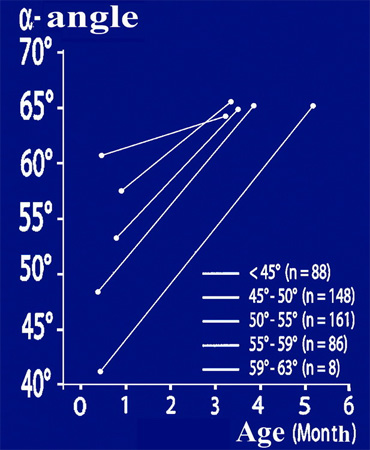 In our group for the study of hip dysplasia we performed several collective statistics, one about the effectivity of different orthoses and ways of treatment. It is shown here, how fast the sonographic alpha angle is improving by a flexion- abduction pillow and later a splint, if treatment begins at the first month of life, even at an angle of 40°. In between 3 and 4 1/2 months the normal mean value of 65° is reached.
In our group for the study of hip dysplasia we performed several collective statistics, one about the effectivity of different orthoses and ways of treatment. It is shown here, how fast the sonographic alpha angle is improving by a flexion- abduction pillow and later a splint, if treatment begins at the first month of life, even at an angle of 40°. In between 3 and 4 1/2 months the normal mean value of 65° is reached.
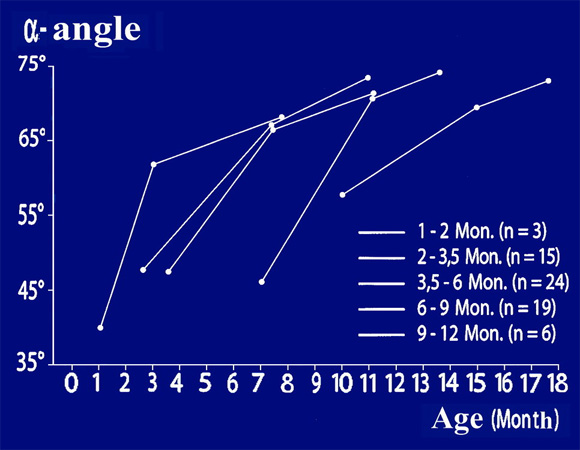 During the first half year and the treatment of hip types 3 and 4 in squatting casts, the alpha angle also showed a steep ascent up to 65°. When the plaster was changed every 6 weeks, we decided after palpating the stability of the joint and controlling the alpha angle, whether flexion-abduction splints would now be sufficient. That was usually possible at an angle of 65° as you see here at the interruptions of the curves.
During the first half year and the treatment of hip types 3 and 4 in squatting casts, the alpha angle also showed a steep ascent up to 65°. When the plaster was changed every 6 weeks, we decided after palpating the stability of the joint and controlling the alpha angle, whether flexion-abduction splints would now be sufficient. That was usually possible at an angle of 65° as you see here at the interruptions of the curves.
The further development according to age was then controlled until showing a normal radiography in the older children. The alpha angle then had reached 72° to 73°. This way a so called residual dysplasia could not develop.
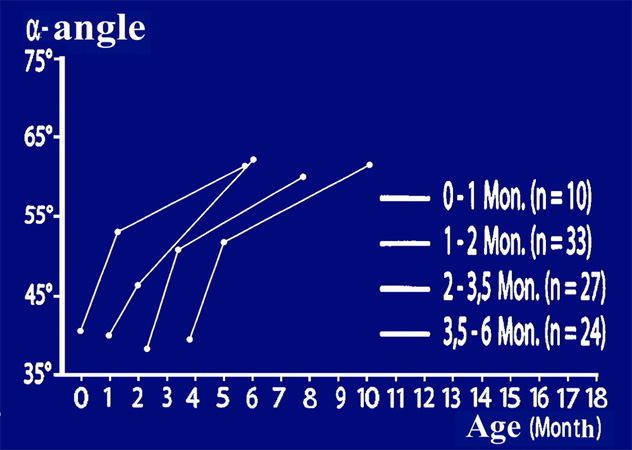 A different result was to be expected, when the plaster cast was applied for one month only, and the change to flexion-abduction splints was allowed at alpha angles in between 46° to 53°; and at 60°, even in type 3 and 4, all therapies were ended. A really normal value at the end, most probably, takes a longer time and needs higher angles.
A different result was to be expected, when the plaster cast was applied for one month only, and the change to flexion-abduction splints was allowed at alpha angles in between 46° to 53°; and at 60°, even in type 3 and 4, all therapies were ended. A really normal value at the end, most probably, takes a longer time and needs higher angles.
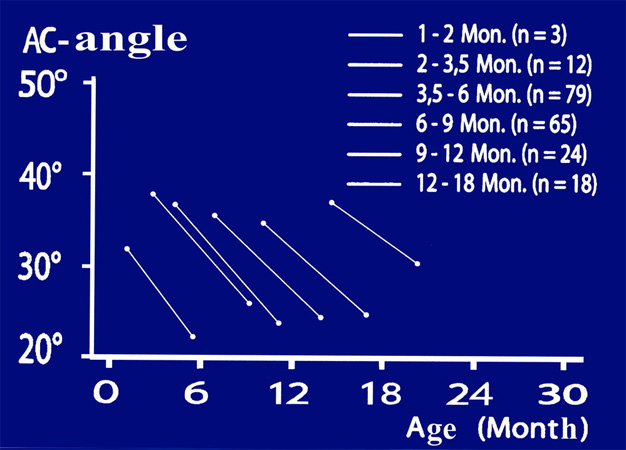 We can realize this, when looking at older curves of dislocations before the introduction of sonography. The radiological acetabular index, during treatment with squatting-cast, improved from 40° to the normal 25° in 6 months. This time is necessary. Today one could of course perform an acetabuloplasty to shorten the time of plastercast of older childen.
We can realize this, when looking at older curves of dislocations before the introduction of sonography. The radiological acetabular index, during treatment with squatting-cast, improved from 40° to the normal 25° in 6 months. This time is necessary. Today one could of course perform an acetabuloplasty to shorten the time of plastercast of older childen.
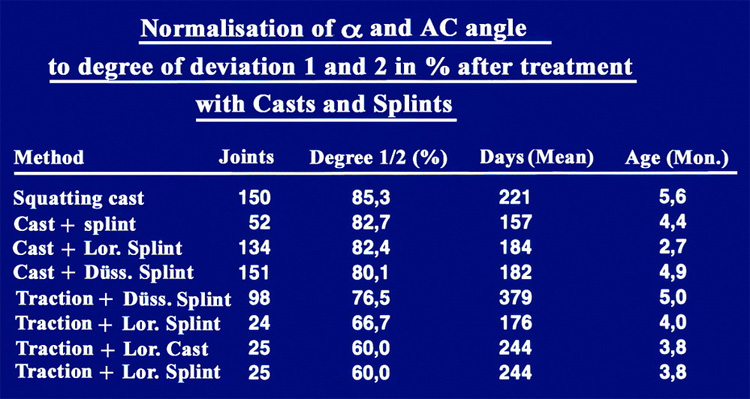 We evaluated the results with our score of normal values and different degrees of deviation from normal to pathological values for the alpha angle and the acetabular index. Children treated only with our squatting-cast, had normal and slightly dysplastic values in 85%; children with additional splints afterwards had 80 to 82.7%. The other methods showed somewhat lower percentages.
We evaluated the results with our score of normal values and different degrees of deviation from normal to pathological values for the alpha angle and the acetabular index. Children treated only with our squatting-cast, had normal and slightly dysplastic values in 85%; children with additional splints afterwards had 80 to 82.7%. The other methods showed somewhat lower percentages.
 For the open reduction of dislocations we changed, after testing the lateral and the medial approach, to an anterior approach in the inguinal crease, No. 2 here.
For the open reduction of dislocations we changed, after testing the lateral and the medial approach, to an anterior approach in the inguinal crease, No. 2 here.
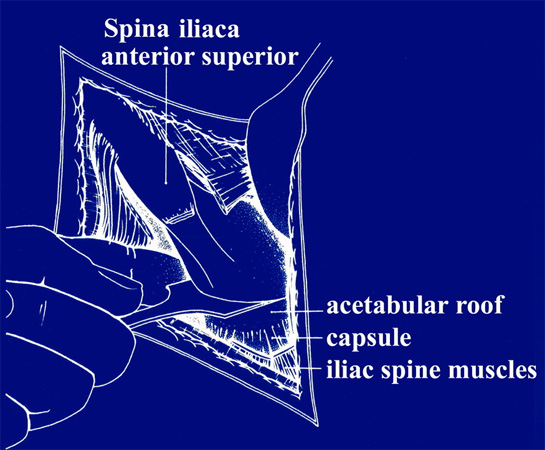
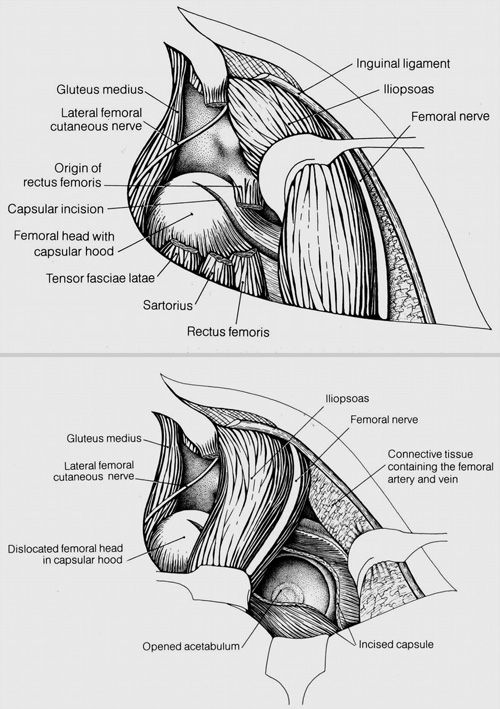 At first (picture top) the femoral head is prepared lateral of the iliopsoas muscle. Then (picture bottom) we pass to the medial side of the iliopsoas and follow him in his fascia to the joint and open it from anterior. Here we have a good vision to the trans-verse ligament, which has to be cut, and to the blood vessels underneath, which have to supply the triradiate cartilage and the three pelvic bones. These vessels should not be traumatized. The reduction of the femoral head is best seen from this approach. Vessels of the femoral head and neck are not touched, since the femoral neck is left covered and the operation is confined to the acetabulum.
At first (picture top) the femoral head is prepared lateral of the iliopsoas muscle. Then (picture bottom) we pass to the medial side of the iliopsoas and follow him in his fascia to the joint and open it from anterior. Here we have a good vision to the trans-verse ligament, which has to be cut, and to the blood vessels underneath, which have to supply the triradiate cartilage and the three pelvic bones. These vessels should not be traumatized. The reduction of the femoral head is best seen from this approach. Vessels of the femoral head and neck are not touched, since the femoral neck is left covered and the operation is confined to the acetabulum.
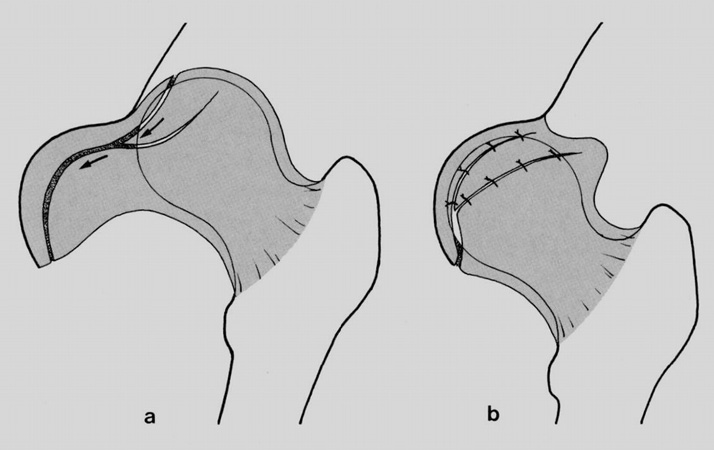 Then a capsulorraphy is performed. The abundant lateral capsule has to be drawn medially, to stabilize the femoral head in the socket. At the same time acetabuloplasties can also be performed choosing the inguinal approach.
Then a capsulorraphy is performed. The abundant lateral capsule has to be drawn medially, to stabilize the femoral head in the socket. At the same time acetabuloplasties can also be performed choosing the inguinal approach.
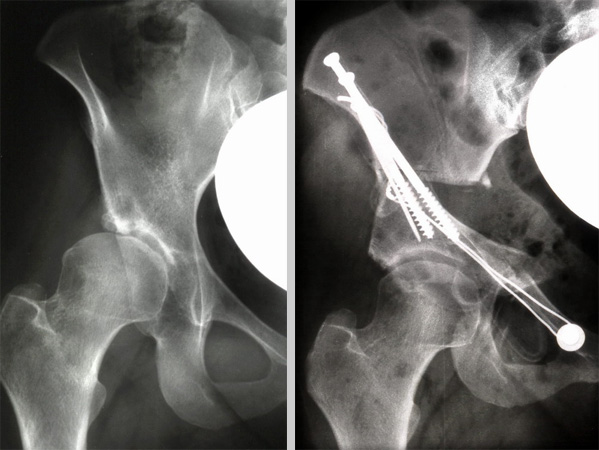
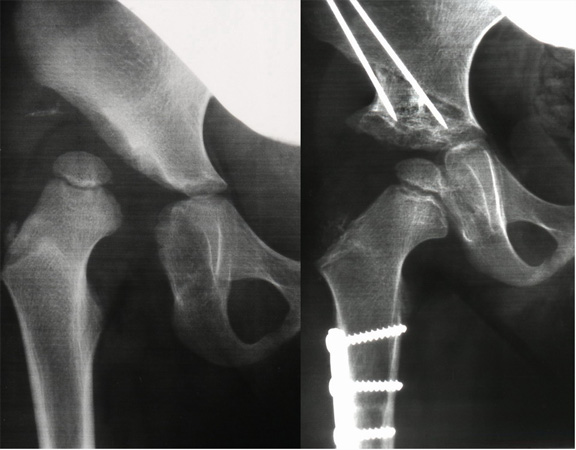 In high dislocations we have to add a subtrochanteric shortening osteotomy at the same time to avoid avascular necroses by increased pressure on the femoral head. The sub-trochanteric osteotomy is easy to fix with a small metal plate of 4 holes because the childen are anyway fixed in the plaster cast.
In high dislocations we have to add a subtrochanteric shortening osteotomy at the same time to avoid avascular necroses by increased pressure on the femoral head. The sub-trochanteric osteotomy is easy to fix with a small metal plate of 4 holes because the childen are anyway fixed in the plaster cast.
83% of our children up to 4 years, with 118 hip joints, could be reinvestigated after 10- 21 years (MV15) together with Cordier. In 78% the CE angle transcended the normal borderline of 25° , and the anterior VCA angle in 83%. Residual dysplasias with CE angles below 20° we found in only 8%, and for the VCA angle in 13%.
Postoperative avascular necroses of grade 1 were seen in 5.9 %, and in grade 2 in only 1.7%; this means we found them mainly in the very low grade 1, and only in a small percentage in grade 2.
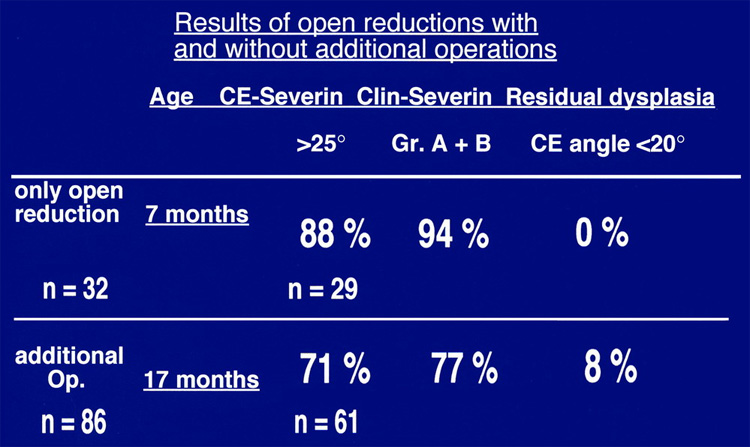 Open reductions alone were performed mainly in the first year of life. At that age no residual dysplasias resulted. In the second year and the following time, additional operations, mainly acetabuloplasties, had to be performed and were still missing in 8%, as just mentioned. This long-time follow-up can be considered as a very good result. After shortening osteotomies there were also no avascular necroses.
Open reductions alone were performed mainly in the first year of life. At that age no residual dysplasias resulted. In the second year and the following time, additional operations, mainly acetabuloplasties, had to be performed and were still missing in 8%, as just mentioned. This long-time follow-up can be considered as a very good result. After shortening osteotomies there were also no avascular necroses.
For a doubtful indication of acetabular osteotomies, our normal values and degrees of deviation can be looked up.
| Age (years/months) |
Grade 1 (normal) |
Grade 2 (slightly pathological) |
Grade 3 (severe pathological) |
Grade 4 (extremely pathological) |
|---|---|---|---|---|
0/3 + 0/4 |
< 30 |
≥ 30 - < 35 |
≥ 35 - < 40 |
≥ 40 |
0/5 - 2/0 |
< 25 |
≥ 25 - < 30 |
≥ 30 - < 35 |
≥ 35 |
2 - 3 |
< 23 |
≥ 23 - < 28 |
≥ 28 - < 33 |
≥ 33 |
3 - 7 |
< 20 |
≥ 20 - < 25 |
≥ 25 - < 30 |
≥ 30 |
7 - 14 |
< 15 |
≥ 15 - < 20 |
≥ 20 - < 25 |
≥ 25 |
 From the different acetabular osteotomies after Albee, Jones, Lance, Salter and Pemberton, we are preferring an almost complete osteotomy of the ilium above the acetabulum, which is good to handle and very effective.
From the different acetabular osteotomies after Albee, Jones, Lance, Salter and Pemberton, we are preferring an almost complete osteotomy of the ilium above the acetabulum, which is good to handle and very effective.
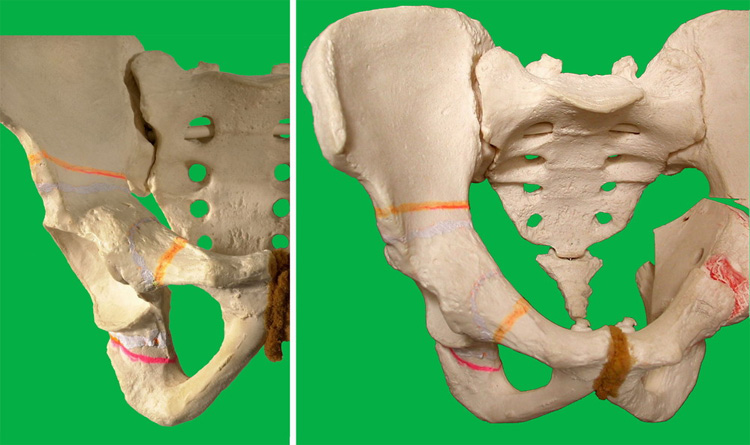
It has been described first by Wiberg in 1953 in the American Journal of Bone and Joint surgery, not by Dega. The acetabular roof is osteotomized under the control of an image intensifier 6-8 mm above the joint from lateral and in our modification until short before the posterior end of the triradiate cartilage. There is a little bony bridge left.
 Anteriorly the osteotomy can be seen all the way. Posteriorly we can palpate the chisel slightly protruding in the greater sciatic notch.
Anteriorly the osteotomy can be seen all the way. Posteriorly we can palpate the chisel slightly protruding in the greater sciatic notch.
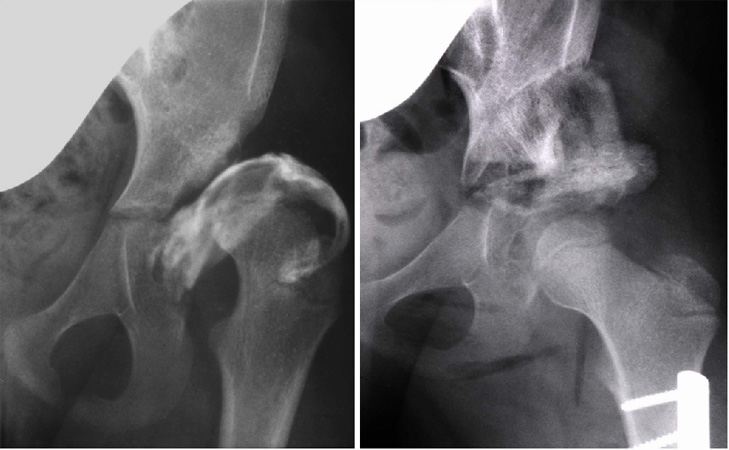 In the little bony bridge between the osteotomy and the triradiate cartilage the acetabular roof is bent down up to 50° as you see here. That is not possible in Salters osteotomy. In this picture the gap above the acetabular roof is filled medially with a triangular bone wedge from the bone bank and laterally with a piece of the femur from the shortening osteotomy.
In the little bony bridge between the osteotomy and the triradiate cartilage the acetabular roof is bent down up to 50° as you see here. That is not possible in Salters osteotomy. In this picture the gap above the acetabular roof is filled medially with a triangular bone wedge from the bone bank and laterally with a piece of the femur from the shortening osteotomy.
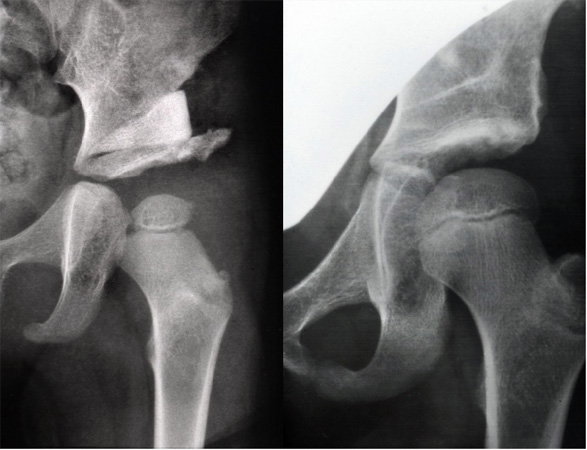 Varus osteotomies and detorsions, as used before, are rarely necessary and do have disadvantages. Earlier and recent reinvestigations have proved this, and here you can see an example of the development as we observe it now.
Varus osteotomies and detorsions, as used before, are rarely necessary and do have disadvantages. Earlier and recent reinvestigations have proved this, and here you can see an example of the development as we observe it now.
 After the age of 10-12 years, rotations of the whole acetabulum are necessary to redirect it in cases of severe dysplasias. Varus osteotomies do not normalize the pathological position of the acetabular roof.
After the age of 10-12 years, rotations of the whole acetabulum are necessary to redirect it in cases of severe dysplasias. Varus osteotomies do not normalize the pathological position of the acetabular roof.
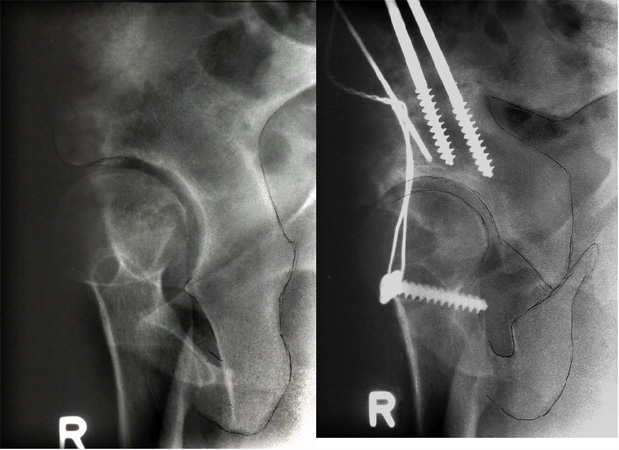
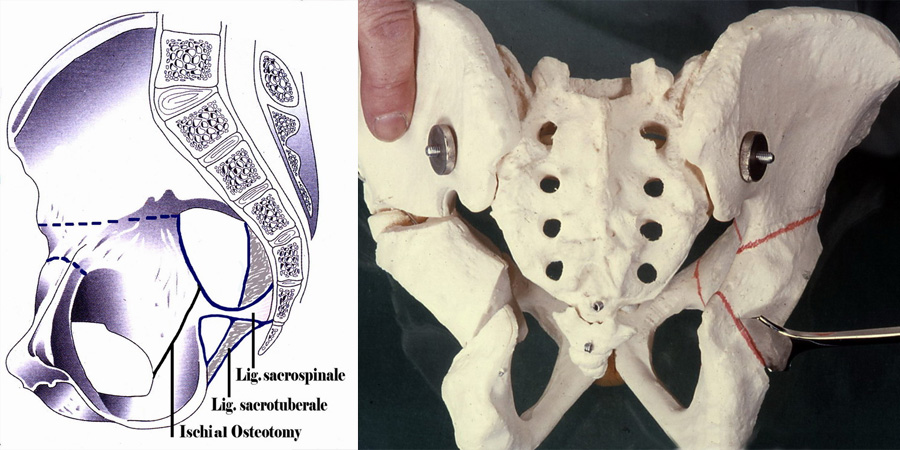 We developed a triple pelvic osteotomy, where the acetabulum is released from the two ligaments, which connect the sacrum and the ischium.
We developed a triple pelvic osteotomy, where the acetabulum is released from the two ligaments, which connect the sacrum and the ischium.
The osteotomy is oblique between the sciatic notch and the obturator foramen. Thus the acetabulum can be rotated freely in three planes, even in severest dysplasias. Otherwise the ligaments will limit all rotations.
When changing the acetabular position, it is necessary, that the acetabular rim is not only bent or levered down laterally and anteriorly, we have to rotate the acetabulum in total. The lateral end, of the osteotomized pubis, should come above the medial end, and be medialized. An osteosynthesis, many years fixed with a wire cerclage, nowadays with screws, is stabilizing the position.
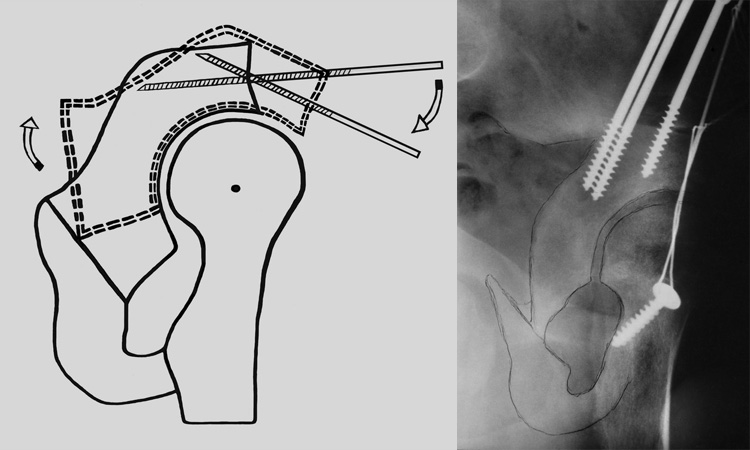 The anterior rotation at its maximum is performed, when the end of the Schanz screw posteriorly is rotated up higher. Otherwise we would shift the acetabulum anteriorly, and the osteotomy would posteriorly show a big gap and be disposed to pseudarthroses.
The anterior rotation at its maximum is performed, when the end of the Schanz screw posteriorly is rotated up higher. Otherwise we would shift the acetabulum anteriorly, and the osteotomy would posteriorly show a big gap and be disposed to pseudarthroses.
 Many colleagues, when seeing that the anterior acetabular margin has come down anteriorly, believe, that this is a good ventral coverage. But it has experimentally been proven by Visser and Anda, and you realize it in the photo at the right, that anterior acetabular rotation will at the same time decrease acetabular anteversion and limit internal rotation of the hip. Therefore, when rotated anteriorly, the acetabulum has, at the same time, to be rotated internally about 10-20 degrees until internal rotation of the hip is normal.
Many colleagues, when seeing that the anterior acetabular margin has come down anteriorly, believe, that this is a good ventral coverage. But it has experimentally been proven by Visser and Anda, and you realize it in the photo at the right, that anterior acetabular rotation will at the same time decrease acetabular anteversion and limit internal rotation of the hip. Therefore, when rotated anteriorly, the acetabulum has, at the same time, to be rotated internally about 10-20 degrees until internal rotation of the hip is normal.
 The anterior rotation is only seen correctly by the "Faux profil" radiography of Lequesne and de Seze.
The anterior rotation is only seen correctly by the "Faux profil" radiography of Lequesne and de Seze.
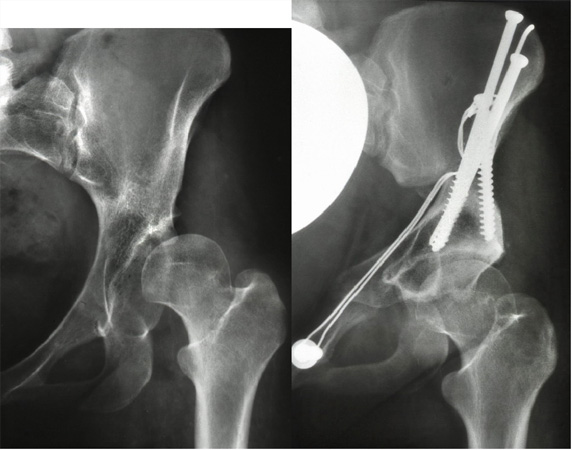 Our goal in the operation is primarily to bring the weight-bearing line into the horizontal position. Almost always, we can achieve this today. A relief of pain is only limited with osteoarthrosis of grade 2 or 3 and an incongruence of femoral head and acetabulum.
Our goal in the operation is primarily to bring the weight-bearing line into the horizontal position. Almost always, we can achieve this today. A relief of pain is only limited with osteoarthrosis of grade 2 or 3 and an incongruence of femoral head and acetabulum.
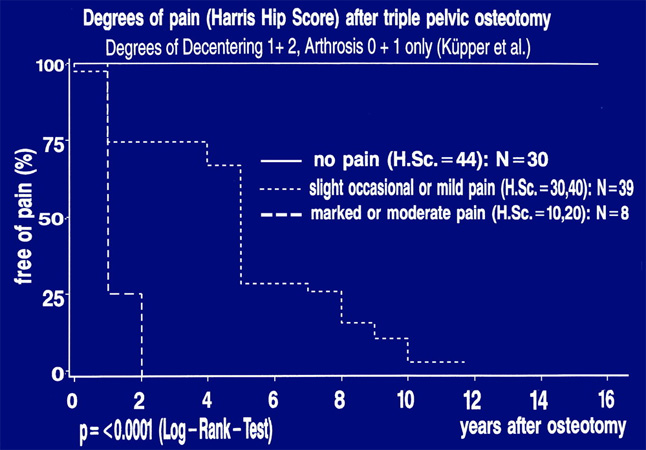 The survivalrate curve of a 10 years reinvestigation, lately performed by Küpper in 77 joints showed, that 30 joints, in the upper line here, were free of pain, 39 below,had a slight or occasional pain and only 8 patients complained of severe pain coming from the spine and iliosacral joints. The hip measurements were normal. False acetabulae and high dislocated joints were excluded in this investigation.
The survivalrate curve of a 10 years reinvestigation, lately performed by Küpper in 77 joints showed, that 30 joints, in the upper line here, were free of pain, 39 below,had a slight or occasional pain and only 8 patients complained of severe pain coming from the spine and iliosacral joints. The hip measurements were normal. False acetabulae and high dislocated joints were excluded in this investigation.
In 1988, when these operations were performed, we did not realize that decreased acetabular and femoral anteversion, when both come close to zero, are the cause of pain, impingement and osteoarthrosis. Probably that is mainly the reason of pain later observed.
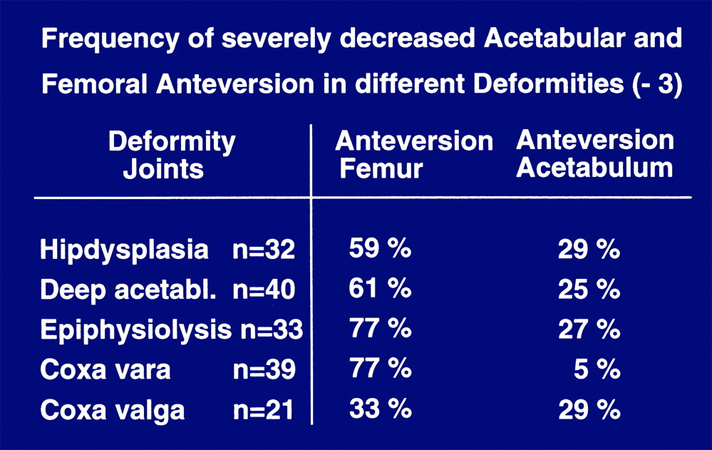 Only in the nineties I evaluated the computertomographies of 356 painful hips. Patients with dysplasia of the hip had in almost 60% an anteversion of the femur close to zero, and in almost 30% an anteversion of the acetabulum close to zero. That was similar in deep acetabuli (CE angle 40-45°) and in 77% also in epiphysiolysis and coxa vara. Today, this third plane has to be considered as well in all patients with arthrosis of the hip and hip dysplasia. Torsional anomalies are quite frequent, but often not diagnosed. When anteversion was corrected up to 15-20°, pain and impingement disappeared.
Only in the nineties I evaluated the computertomographies of 356 painful hips. Patients with dysplasia of the hip had in almost 60% an anteversion of the femur close to zero, and in almost 30% an anteversion of the acetabulum close to zero. That was similar in deep acetabuli (CE angle 40-45°) and in 77% also in epiphysiolysis and coxa vara. Today, this third plane has to be considered as well in all patients with arthrosis of the hip and hip dysplasia. Torsional anomalies are quite frequent, but often not diagnosed. When anteversion was corrected up to 15-20°, pain and impingement disappeared.
Ladies and gentlemen, we have chosen these ways of diagnosis and therapy after a long period of research. I can recommend them now as optimal.
| Download | |
|---|---|
| Diagnosis and Treatment of Developmental Hip Dysplasia – Our Experience | PDF (8.2MB) |