Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Epidemiology and Classification of DDH and Torsional Deviations of the Hip Joint
© Prof. Dr. med. Dietrich Tönnis, Dr. med. Achim Heinecke
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
Developmental hip dislocation is the most frequent deformity at birth. Grill reported from the Austrian hip screening program a rate of sonographically pathological hips of 6.57%. In the newbornscreening of our hospital Storch found 2.64%. And when later deteriorating 2a hips were added, it summed up to also 6.14% (Tab. 1 and Tab. 2).
| Hip types of Graf | % |
|---|---|
| 2c | 1.2 |
| 2d | 0.9 |
| 3a | 0.5 |
| 4 | 0.04 |
| 2.64% |
| 2a to 2a - | 7.9% |
| 2a to 2c | 1.0% |
| 8.9% |
The deformity we are speaking of, was first called CDH: Congenital dislocation of the hip, because it was noted at birth or sometimes later. Then the term DDH was introduced: Developmental dislocation of the hip, because it developes during growth under external forces, first in the uterus, and later, if it is not treated.
Partly it was differentiated between dysplasia, subluxation and dislocation. Also the directions of dislocations in the beginning were used for classification: Anterior, lateral and posterior dislocation.
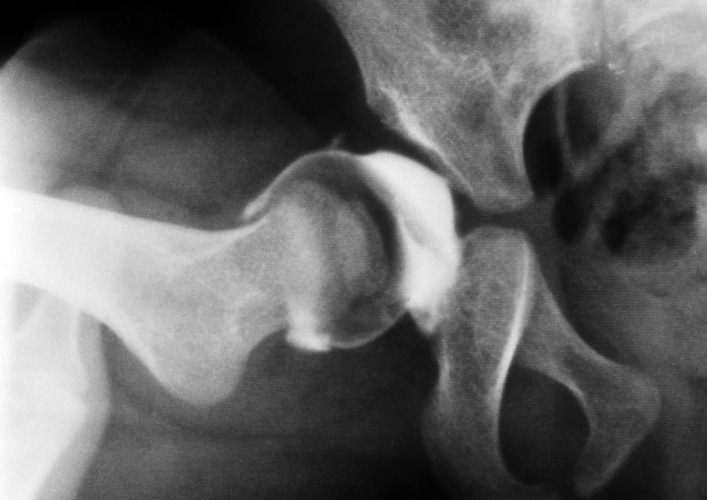
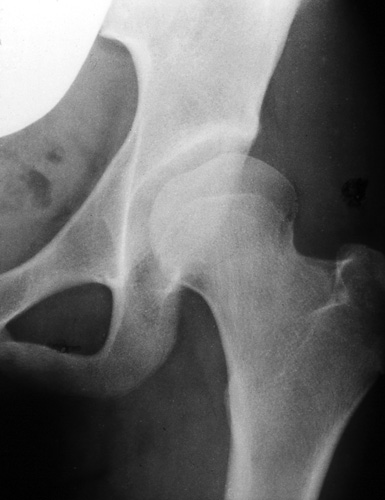
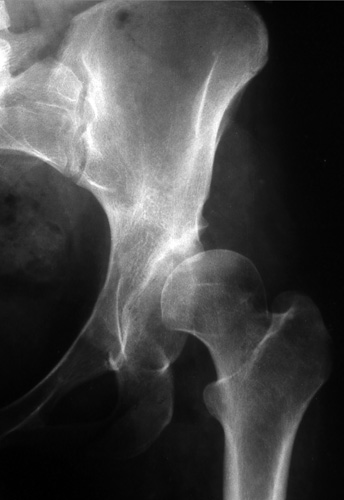
Most frequently there is a proximal lateral and anterior decentration, as seen here in the ap and the lateral view of Lequesne and de Seze (Fig. 1 and Fig. 2). Only very high dislocations are found posteriorly of the pelvic wing.
The typical attribute of a dislocated hip is instability. This we can palpate or observe with sonography or arthrography (Fig. 3). Here the femoral head is pushed laterally by my thumb in a one year old child and in Fig. 4 it is reduced into the joint.
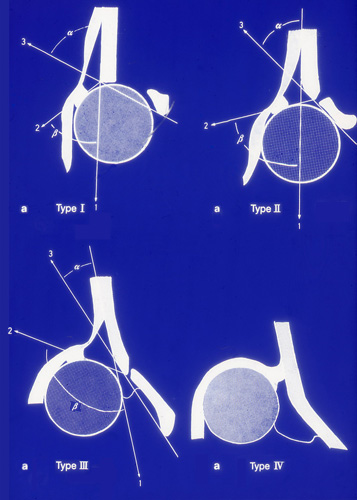
This is found also in Grafs hip types 2b and c in Fig. 7. In the lower line you see his partial dislocation typ 3 at the left and at the right the full dislocation.

In the arthrogram at Fig. 8 a typ 3 hip is shown. The contrast fluid is filling the acetabular cavity and the femoral head is displaced, but has pulled the labrum with it.
 In Fig. 9, in a position of increased flexion and abduction, the femoral head is almost completely reduced. The lower labrum and transverse ligament are only minimally protruding.
In Fig. 9, in a position of increased flexion and abduction, the femoral head is almost completely reduced. The lower labrum and transverse ligament are only minimally protruding.
In Fig. 10, the femoral head has passed acetabular rim and labrum and in Fig. 11 the capsule is constricted. This is what Leveuf and Bertrand 1937 already called the true and complete dislocation and it is Grafs typ 4 hip. Howorth (1960) and similarly Dunn (1969) have also described these types of hips.
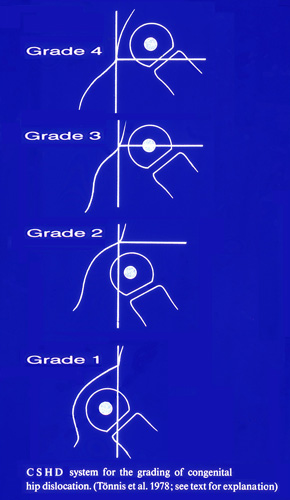 For a radiological classification and evaluation of results we introduced these grades (Fig. 12). They express where the femoral head center, or its ossific nucleus, stands in relation to the acetabular rim.
For a radiological classification and evaluation of results we introduced these grades (Fig. 12). They express where the femoral head center, or its ossific nucleus, stands in relation to the acetabular rim.
Below, at grade 1, it stands medial of Perkins and Shents vertical line from the acetabular rim. At grade 2 the center stands lateral of the line, but still below the acetabular rim, at grade 3 - at the height of the rim, and and at grade 4 –above it.
For the evaluation of triple pelvic osteotomies we separated 4 degrees of decentration of the femoral head, which will show different results at longer follow-ups. Grade 1 (Fig. 13) classifies spherical and well reduced joints, but the femoral head is not fully covered. These joints have a quite normal congruence of femoral head and acetabulum before and after operation and should have the best long-time follow-ups.

Grade 2 (Fig.14) is characterized by an elongated dysplastic acetabulum and the femoral head is shifted proximally. Yet, postoperatively it also looks quite congruent now. The femoral head is deeper reduced into the socket here.
Grade 3 (Fig. 15) classifies the false acetabulum. Here the femoral head has itself molded a secondary acetabulum. The definition is, that the femoral head is stable in this relatively short and shallow cavity.

A grade 4 (Fig. 16) was chosen in addition for high dislocated femoral heads, that can still be reduced into the acetabulum by abduction. We have to proof on abduction whether the femoral head can be brought more into the joint and acetabular rotation can cover it. The weightbearing area however will still be smaller than in normal joints.
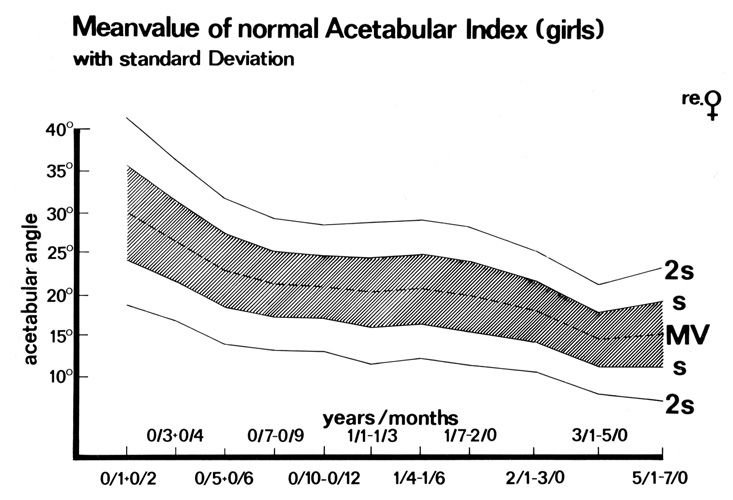 Another classification of the joints and their pre- and postoperative state can be given by measurements of angles and indices (Fig. 17). Our investigation of the normal acetabular index in children by a follow-up to the age of 7 years is well known I believe (Tönnis u. Brunken 1968).
Another classification of the joints and their pre- and postoperative state can be given by measurements of angles and indices (Fig. 17). Our investigation of the normal acetabular index in children by a follow-up to the age of 7 years is well known I believe (Tönnis u. Brunken 1968).
| Age (years/months) | Normal value (mean) | Grade 1 (normal) | Grade 2 (mildly pathological) | Grade 3 (moderately pathological) | Grade 4 (extremely pathological) |
|---|---|---|---|---|---|
| 0/3 + 0/4 | 25 | < 30 | ≥ 30 - < 35 | ≥ 35 - < 40 | ≥ 40 |
| 0/5 - 2/0 | 20 | < 25 | ≥ 25 - < 30 | ≥ 30 - < 35 | ≥ 35 |
| 2 - 3 | 18 | < 23 | ≥ 23 - < 28 | ≥ 28 - < 33 | ≥ 33 |
| 3 -7 | 15 | < 20 | ≥ 20 - < 25 | ≥ 25 - < 30 | ≥ 30 |
| 7 -14 | 10 | < 15 | ≥ 15 - < 20 | ≥ 20 - < 25 | ≥ 25 |
We have then inroduced, in addition to the normal values for each age, degrees of deviation, a grade 2 mildly pathological, degree 3 severly and degree 4 extremely pathological (Tab. 3). In this way we can count how many joints are pathological and to what degree before operation and afterwards. To achieve normal values is the best way to achieve good long-time results.
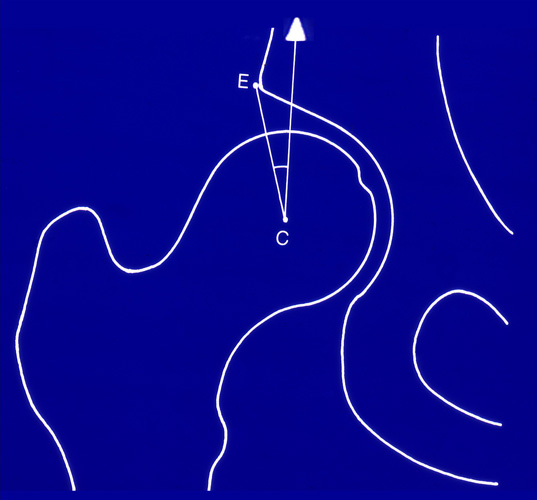
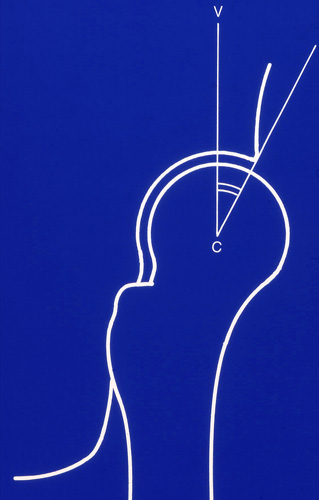
Important angles are Wibergs CE angle of the lateral coverage of the femoral head (Fig. 18), then the VCA angle of the anterior coverage of Lequesne and de Seze (Fig. 19, 20).
Important angles are Wibergs CE angle of the lateral coverage of the femoral head (Fig. 18), then the VCA angle of the anterior coverage of Lequesne and de Seze (Fig. 19, 20).
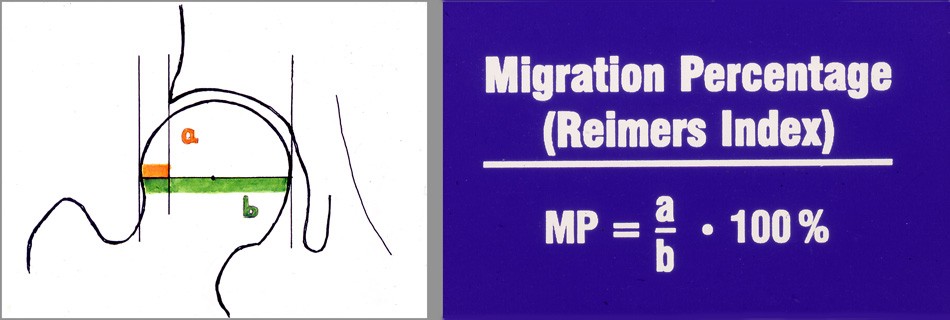
At the weightbearing loading zone of Bombelli the joints presented with 74% the highest percentage free of pain at an angle of -5° to +5° , so practically at horizontal coverage. At the migration percentage, at 10-15% uncoverage, 87.9% of the joints were free of pain. But at 5% above and below, the percentage dropped immediately.
In this way we also investigated the other normal angles and found 30-35° as optimal for the Wibergs CE and VCA angle. A borderline of 25° seems too deep. But we have also to realize that overcorrection of acetabular rotation can create a deep acetabulum that also causes pain. Therefore these values should be kept in mind.
In our first long-time follow-up of triple pelvic osteotomies (1994) we correlated the absence of pain with the different angle groups (Tab. 4).
| CE angle | 30 - 35° |
| VCA angle | 30 - 35° |
| Loading zone angle | -5 to +5° |
| Migration (%) | 10 - 15 |
For the adults we have now this list of normal values and the degrees of deviation to quantify our results (Tab. 5).
| Degrees | 1 (normal) |
2 (mildly pathological) |
3 (severely pathological) |
4 (extremely pathological) |
|---|---|---|---|---|
| MP: migration percentage; LCE: lateral CE angle (Wiberg); ACE: anterior CE angle (Lequesne and de Seze); WBZ: weightbearing zone angle (Bombelli) | ||||
| LCE | ≥ 30 | 20 -29 | 5 - 19 | < 5 |
| ACE angle | ≥ 25 | 20 -24 | 5 - 19 | 30 - 35° |
| WBZ angle | ≥ 9 | 10 -15 | 16 -25 | > 25 |
| Reimers (MP) | ≥ 15 | 16 -25 | 26 - 40 | > 40 |
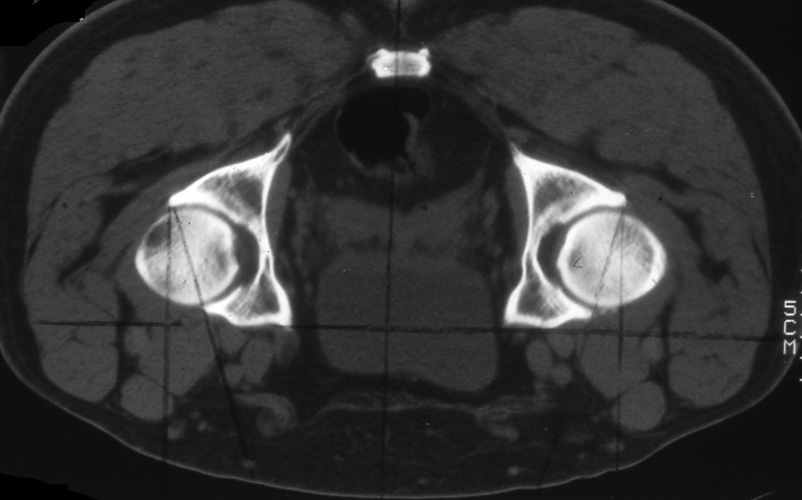 So far we have considered only the classifications of two planes of the hip joint. By computertomographies in prone position to equalize pelvic inclination (tilt) we get pictures of the horizontal or axial plane, in which we can measure the anteversion of the acetabulum and the femur, as seen in Fig. 23.
So far we have considered only the classifications of two planes of the hip joint. By computertomographies in prone position to equalize pelvic inclination (tilt) we get pictures of the horizontal or axial plane, in which we can measure the anteversion of the acetabulum and the femur, as seen in Fig. 23.
In 1999 we published the femoral and acetabular anteversion in computertomographies of 256 hips of adolescents and adults with pain at the hip joints
(Tönnis u. Heinecke).
| Grade -3 | < 10° | AA and FA severely decreased |
| Grade -2 | 10 - 14° | Moderately decreased |
| Grade 1 | 15 - 20° | Assumed normal range |
| Grade +2 | 21 - 25° | AA and FA slightly increased |
| Grade +3 | > 25° | Severely increased |
Anteversion angles of 15 - 20° were assumed as normal in acetabular and femoral anteversion and tested during the investigation as group 1. Decreased angles were divided in group -2 and -3 and increased angles in group +2 and +3. A severely decreased anteversion has angles below 10°, a moderately decreased angles between 10 and 14° (Tab. 6).
 The decrease of anteversion was either developmental from birth and childhood or going along with a coxa vara or an asymptomatic moderate slip of the capital femoral epiphysis. Hip dysplasia with a CE angle below 20° was evaluated separately, also the deep acetabulum and protrusio acetabuli.
The decrease of anteversion was either developmental from birth and childhood or going along with a coxa vara or an asymptomatic moderate slip of the capital femoral epiphysis. Hip dysplasia with a CE angle below 20° was evaluated separately, also the deep acetabulum and protrusio acetabuli.
Acetabular and femoral anteversion can be combined in a joint quite differently. When both are decreased or increased, the deformation is worse.
When decreased and increased angles are combined, a compensation is seen. McKibbin has described an instability test, in which he counted the degrees of acetabular and femoral anteversion together.
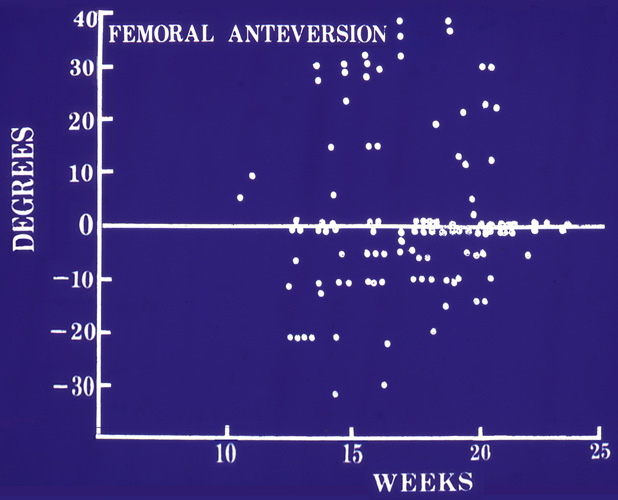
At 50 - 60 degrees there was a marked instability in the joint. We introduced here the normal angle group and the deviation degrees by doubling the angles. This is the classification of the third plane of the hip joint. The frequency of the groups during the first half year of life. is seen in Fig. 24.
Decreased anteversion of acetabulum and femur is much more symptomatic, than increased anteversion. But it is mostly not diagnosed.
| Index | Joints | Rotation | Mean value | p-Wilcoxon |
|---|---|---|---|---|
| < 20 | 82 | IR / ER | 17.2° / 46.0° | < 0.001 |
| 20 - < 30 | 40 | IR / ER | 17.9° / 39.1° | < 0.001 |
| 30 -40 | 35 | IR / ER | 33.3° / 36.1° | 0.0414 n.r. |
| > 40 | 32 | IR / ER | 42.3° / 36.7° | 0.161 |
Typical for decreased anteversion of acetabulum and femur is the decrease of internal rotation of the hip and the increase of external rotation (Tab. 7). In further investigations we found also a correlation between decreased anteversion index groups and pain and osteoarthrosis .
In symptomatic and asymptomatic SCFE (Slipped capital femoral epiphysis) femoral anteversion was decreased in total to 90.3%. 77% of these joints showed the extreme decrease of group -3. In 48%, a severe or moderate decrease was also present in the acetabular anteversion.
Coxa vara shows also a very high percentage of severe decrease of femoral anteversion with practically 77 % for group -3, coxa valga only in 33.3 %. But this is anyway amazing. We would not expect a reduced femoral anteversion in a coxa valga.
At hip dysplasia in almost 60% the femur showed also a -3 degree of anteversion and the acetabulum in 29%. So far increased anteversion was more expected in DDH, but that was minimal among the patients with pain at the hip.
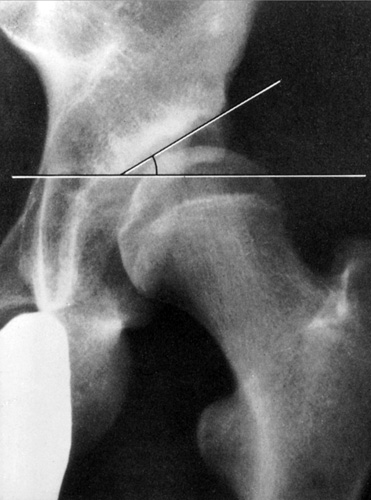
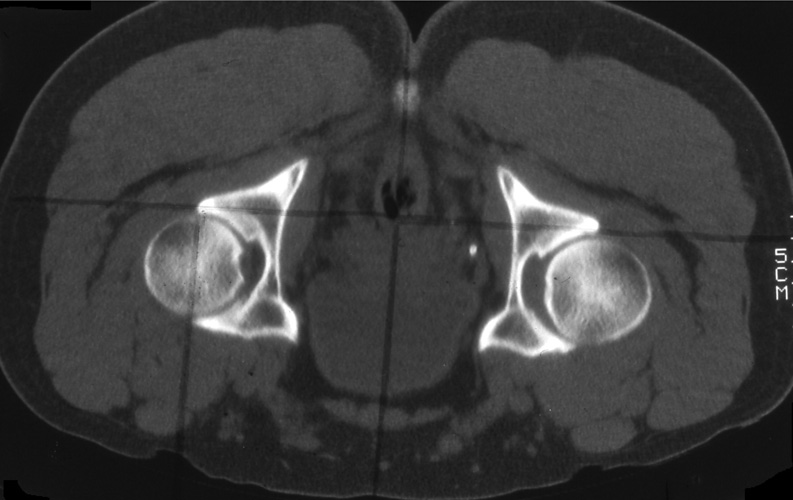 The techniques of measuring should be looked up in our special papers on torsional anomalies of the hip. A short example is given in Fig. 25.
The techniques of measuring should be looked up in our special papers on torsional anomalies of the hip. A short example is given in Fig. 25.
Anteversion is here measured only at the right hip. It is zero. Here the anterior acetabular rim has a normal length and congruency. This is not seen at the left hip. Here the femoral head is cut at a lower level where the anterior acetabular rim is receding more and more and measuring would be wrong.
| Download | |
|---|---|
| Epidemiology and Classification of DDH and Torsional Deviations of the Hip Joint | PDF (6.9MB) |