Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Flexion Osteotomies of the Fermoral Neck to bring round posterior remainders of the femoral head in Legg-Calvé-Perthes Disease into the weight bearing position - A New Technique
© Prof. Dr. med. Dietrich Tönnis, Dr. F. Tewes, Dr. A. Heinecke
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
Abstract
The flat femoral heads in Legg-Calvé-Perthes disease so far have been treated operatively by varus osteotomies, hoping that the acetabular roof will form the femoral head round again during growth, when it is more covered. But the results are limited and even worse with increasing age.
Catterall (3, 4) has described that the avascular necrosis starts from below ventrally up to the top and then down posteriorly. The arterial vessels have a circular system below at the femoral neck and send vessels anteriorly and posteriorly up to the top of the femoral head.
Catterrall divided the patients in 4 groups. We have found that the groups 1, 2, 3 and to some degree even 4 have residual round femoral heads. They can be rotated by a flexion osteotomy into the weightbearing plane. Then we get again congruently covered femoral heads. The radiographies and measurements are much better then and normal in a high degree.
The roundness of the femoral head Mose (12) has measured in 4 degrees of deviation. 69% of the children had postoperatively a round surface of grade 1 and 2. Catterall group 3 reached a maximum of Mose grades 1 and 2 in 81%, group 2 in 66.6%, group 4 in 57.1%.
The age-group of 10 years and more came to Mose grades 1 and 2 in 81.8%, the children 6-10 years old in 65%, the children less than 6 years of age in 63.6%.
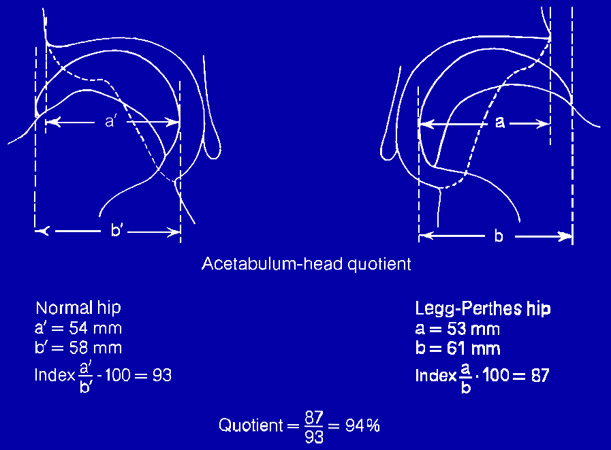
Further angles of the depth of the acetabulum and the outside Acetabulum-Head-Quotient (6 ,7) were measured .The breadth of the dislocation of the hip in the epiphysis postoperatively reached the grades 1 and 2 in 95.5%.
Introduction
Einleitung
Currently the operative treatment of the Legg-Calvé-Perthes disease has utilised the principle of “Containment“.
In 1952 Soeur and de Racker (8) used a varus osteotomy of the upper femur to rotate flat and subluxating femoral heads into the acetabulum with the hope that this would lead to remodel. Acetabuloplasties,
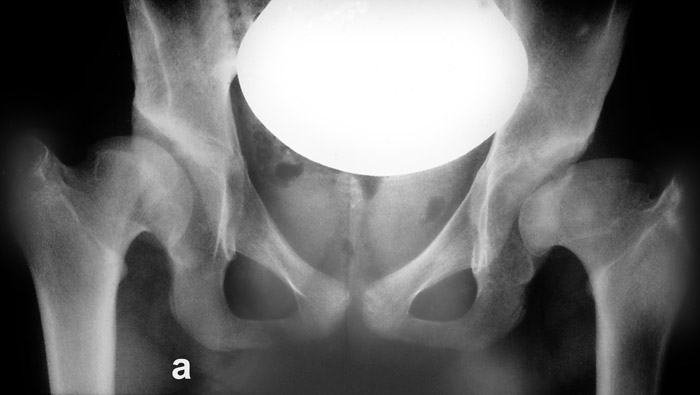
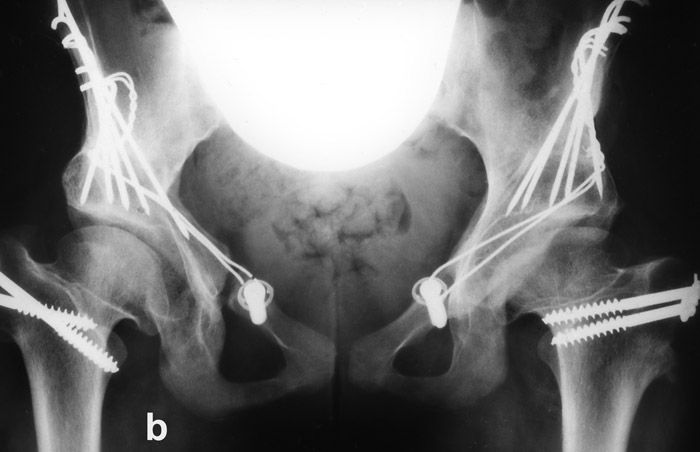
Salter and Chiari osteotomies and finally triple pelvic osteotomies were tried (Fig. 1a, b). In a number of patients , however, the acetabulum became flatter as the result of treatment (9 and 10). This may be the reason for less good results of operations in older children (5).
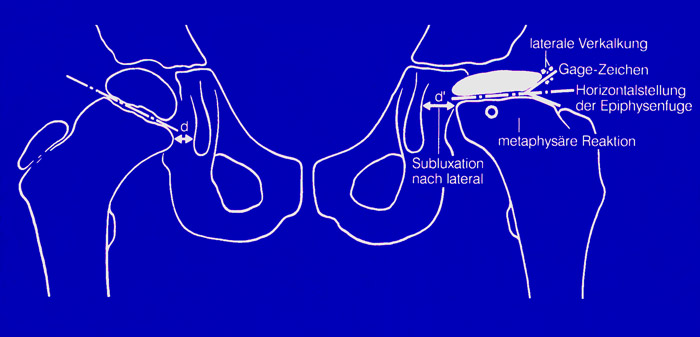
The area of necrosis extends from anterior to the top of the femoral head and then posteriorly. Catterall (1, 4) has described that it develops in 4 steps. First a small area lies in front below (group1). The second one extends from there up to the top from ventral as group 2. Then the following step (group 3) is reaching from the top down at the dorsal side but leaving below the last, the posterior part of the femoral head as group 4.
Once we had an adult patient with a small cyst in the anterior part of the femoral head. She complained of pain only when he went upstairs and bend her body anteriorly. We performed used a flexion osteotomy of the femoral neck to bring the posterior part of the femoral head into the weight bearing plane and her pain was gone. This gave us the idea to perform flexion osteotomies in children, when they suffered from osteonecrosis of the anterior parts of the femoral head in Legg-Calvé-Perthes disease.
Additionally we rotate the femoral neck anteriorly until the range of internal rotation is greater than the range of external rotation We make reference to our papers on the decreased anteversion of femur and acetabulum in the aetiology of osteoarthritis of the hip (23, 24).
In this paper we want to present our results of flexion osteotomies. Frequently, however, varus osteotomies were also performed in addition, when there was a subluxating coxa valga and a very short flat acetabulum.
The orthograde, straight lateral radiography
To examine the femoral anteversion, today, the lateral radiography of the femur is frequently performed after Lauenstein (13) in a position of only 70° instead of 90° flexion and about 50° of abduction. This is actually an oblique radiography.
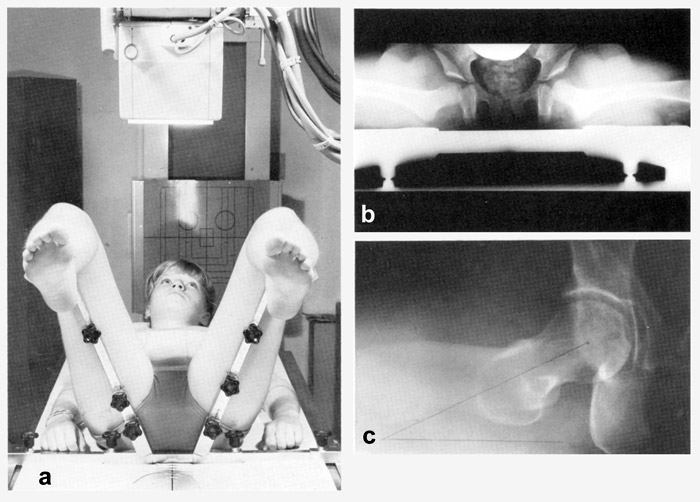 Dunn (6) and mainly Rippstein (14) developed a positioning apparatus (Fig. 2a, b, c). In small children both hips are depicted on one film (Fig. 2a). In adults we take separate axial views of each hip (Fig. 2c).
Dunn (6) and mainly Rippstein (14) developed a positioning apparatus (Fig. 2a, b, c). In small children both hips are depicted on one film (Fig. 2a). In adults we take separate axial views of each hip (Fig. 2c).
The legs are flexed exactly 90° at the hips and knees (Fig. 2c). The lower legs are parallel to the sides of the table to eliminate any medial or lateral rotation of the hip and the thighs. They are perpendicular to the table. The hips are abducted 20°.
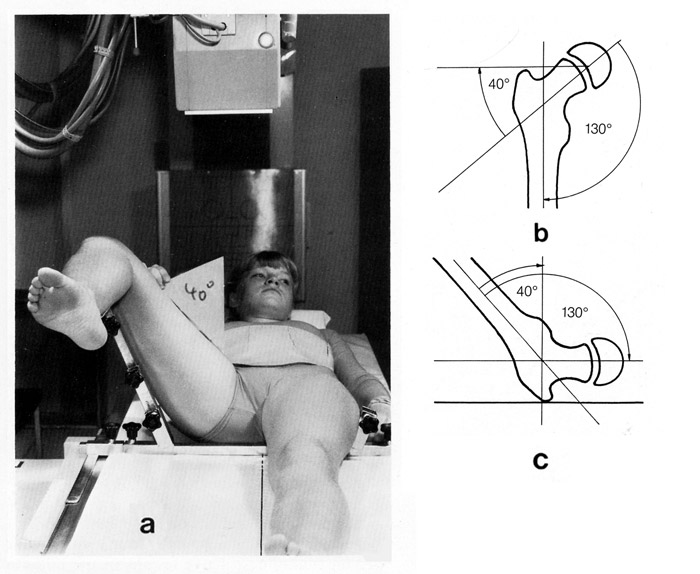 Imhäuser (10) has described, what he called an “orthograde lateral x-ray“, where the radiography is vertical. (Fig. 3a, b, c). The abduction should be: femoral neck angle minus 90°. That means, at 130° the leg should be abducted 40° and at 140° it should be 50°. Then the femoral neck is lying flat on the table for radiography and the femoral neck can be seen exactly from lateral and especially with the posterior part.
Imhäuser (10) has described, what he called an “orthograde lateral x-ray“, where the radiography is vertical. (Fig. 3a, b, c). The abduction should be: femoral neck angle minus 90°. That means, at 130° the leg should be abducted 40° and at 140° it should be 50°. Then the femoral neck is lying flat on the table for radiography and the femoral neck can be seen exactly from lateral and especially with the posterior part.
Indication for Operation
Operations were performed when there was a marked flattening of the femoral head. In quite a few patients with additional subluxations of the femoral head a varus osteotomy was added. Also the femoral anteversion was corrected, if it was decreased and internal rotation limited (23, 24). The age groups were first below 6 years, then 6 to 10 years and then above 10 years.
Technique of Operation
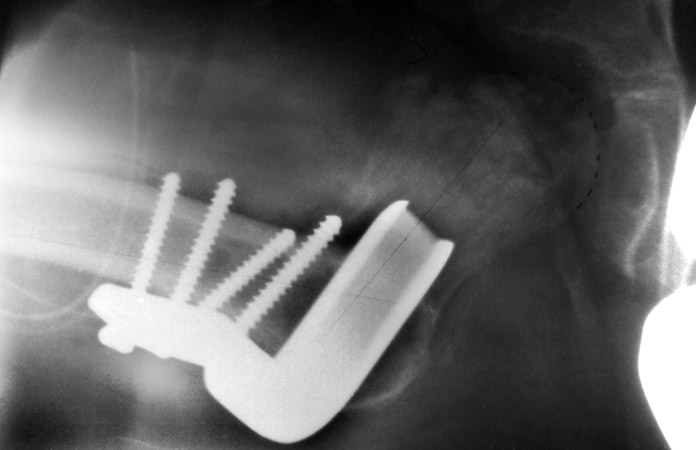
Flexion osteotomies were performed intertrochanterical with the control of the image intensifier. In some cases valgus osteotomies were necessary to increase femoral anteversion, which frequently was low. External rotation contractions were often encountered. To correct this, the distal femur was rotated, so that the internal rotation of the hip was 15-20° higher than the external. As a result the flexion angle was increased too. This was also the way to avoid osteochondrosis as we mentioned already (23, 24).
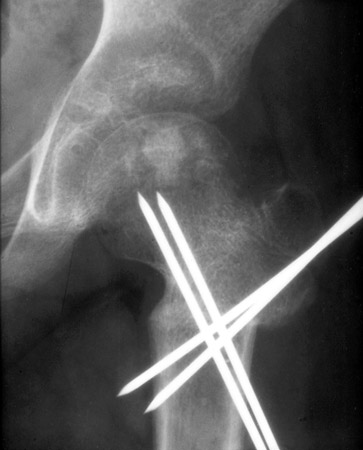
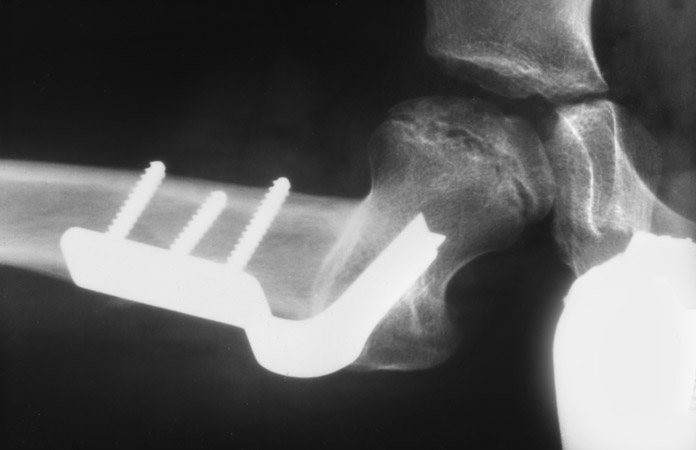
The osteotomies in very small children where fixed with K-wires, in the elder ones with plates with screws. After operation a hip spica was given for 6-8 weeks until the osteotomy was stable. The figures 8, 14, 19, 22, 26, 33 and 36 are showing the final results - a round femoral head apt for weight bearing.
Material
42 children, 28 boys and 14 girls came for reinvestigation. Children with the disease on both sides or additional acetabuloplasties were not included. In 22 hips the right hip was concerned, in 20 the left. 3 joints with additional acetabuloplasties were also not included.
11 children were younger than 6 years, 20 were 6-10 years and 11 more than 10 years old. Since our flexion osteotomies show good results even in older children, this group is greater than in other statistics. The follow-up time ranged from 1 to 8 years, in average 3.1 years.
The number of femoral osteotomies was different:
Flexion and Anterotation3 joints
Flexion and Valgus Osteotomy2 joints
Flexion, Valgus Osteotomy, Anterotation4 joints
Flexion and Varus Osteotomy14 joints
Flexion, Varus Osteotomy, Anterotation19 joints
Osteonecrosis was preoperatively seen in different percentages:
Beginning necrosis8%
Advanced necrosis28%
Beginning of recovering2%
Advanced recovering2%
The majority was operated rather late. But the flexion osteotomy still offers good or fair results, although the early results above 10 years opposite to the younger children.
A simple classification for the form of the femoral head was introduced:
Femoral head round6
Femoral head moderately flat21
Femoral head very flat15
The serious deformities are also seen in the tables of the measurements after Mose (12, 13) in the Catterall groups 3 and 4 (Tab. 4). Group 3 had the most patients with 21. 52.4% recovered to grade 1 and 28.6% to grade 2, together 81%, a very good result. But group 4 with the minimal rest of the femoral head was also considerable with 57.1% at grade 1 and 2 of deviation. It may be of importance that the posterior side of the femoral head has the best vascular nourishment.
Table 5 shows the improvement of the Mose grades in different groups of age. Grade 1 and 2 added were found in children under 6 years in 63.6%. At the age between 6 and 10 years in 65% and above 10 years in 81.8% astonishingly.
Clinical results
Pain
90.7% of the joints at reinvestigation were free of pain, 9.3% had grade 1 of pain only at longer walking.
Ability of walking
85.0% of the patients had no limit at walking (grade 1). 12.5% felt pain when walking more than 1 hour (grade 2), 2.5% had pain after walking up to 1 hour (grade 3).
Sign of Trendelenburg
60% of the patients had no limping of the pelvis when standing on one leg only (grade 0). 32% - when tired at longer walking - noticed a limping or instability when standing longer on one leg (grade 2). 5% steadily had a slight limping (Grade 3), 2.5% a marked limping (grade 3).
At the flexion and the varus osteotomy a slight limping is frequently seen because the mayor trochanter is standing higher now and the gluteus muscles are relaxed then. But by further growth limping diminishes. Some children were reinvestigated a short time after operation.
Range of Movement
The range of movement of the hip increased in all directions. There remained no flexion contracture. By the rotation, osteotomies, the inequality of external rotation of 39.5° and decreased internal rotation to 24.4° was corrected to prevent impingement and osteoarthrosis (12). The internal rotation then was 38.5°, the external 36.3°.
Material of Radiographies
Pictures of the development of our children are probably more convincing than many statistics. Therefore we place this chapter of seven patients first.
Fig. 4 shows a flat, laterally cornered femoral head of a 10 years old boy. Fig. 5, the straight lateral radiography, presents a severe osteonecrosis up to the dorsal parts of the femoral head.
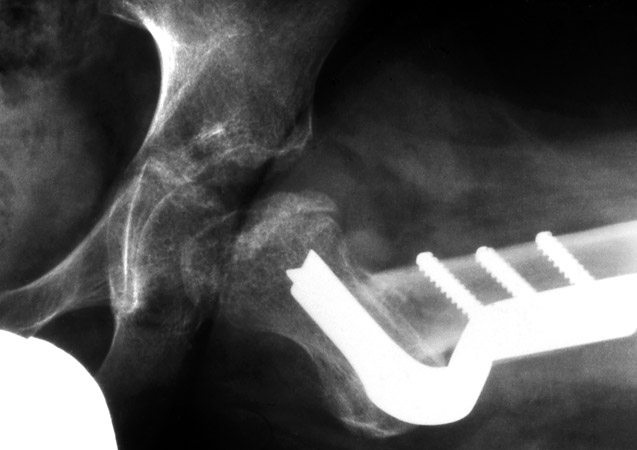
In Fig. 6 we can see at the angled hip plate how much the femoral neck was flexed anteriorly.
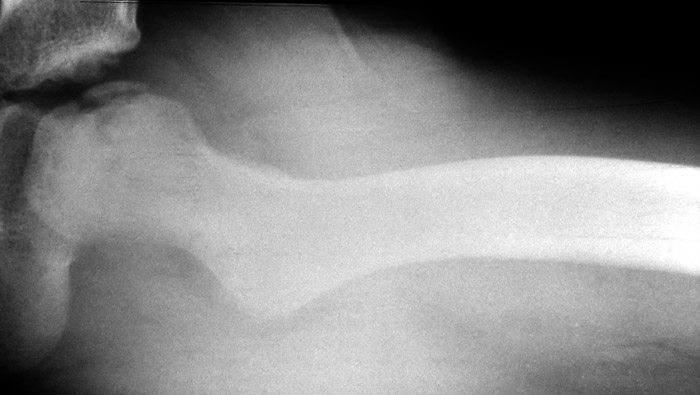
It is shown also 4 years later in Fig. 7. Here the round posterior part of the femoral head is presented.
The anterior (a.p.) picture (Fig. 8) at the same time shows a hip joint of a normal congruence. Only in anteversion of the acetabulum is somewhat decreased.
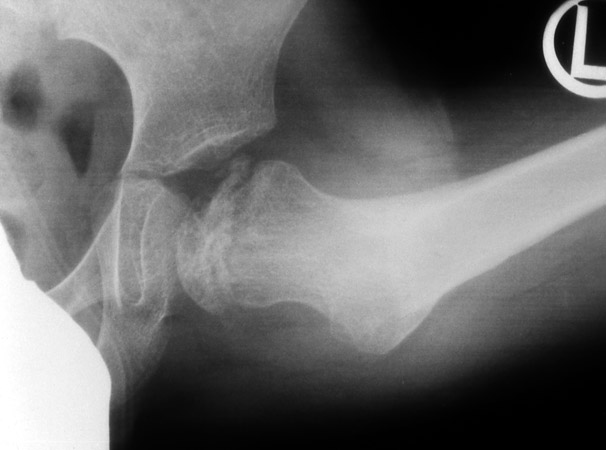
Fig. 9 is belonging to an 11 years old girl. The lateral x-ray (Fig. 10), which she brought with her, is twisted and performed after Lauenstein. It seems that only the posterior part is still present.
The flexion osteotomy, but also a varus correction was performed (Fig. 11). A straight lateral x-ray was made only 6 years later (Fig. 12). The strong flexion osteotomy and the dorsal rest of the femoral head are shown. It seems to be in between Catterall grade 2 and a part 3 is left.
The radiographics 3 years later (Fig. 13) and 8 years later (Fig. 14) show a good position of the rest of the femoral head in the acetabulum. The additional varus osteotomy here was necessary.
Fig. 15, 16 and 17 show the radiographies of an 8 years old girl. It is difficult to say which degree of Catterall is present here. After 2 1/2 months, when a straight lateral view was taken, grade 2 and a part of 3 is involved.
But the rest of 3 and a good part of 4, brought into the weight baring plane, are taking the weight (Fig. 18). The ventral flexion of the femoral neck is considerable. The last picture, (Fig. 19) about 5 years after operation shows a normal hip, almost incredible.
The pictures of Fig. 20 were taken from an almost 8 years old boy. The straight lateral picture (Fig. 21) still shows a part of the dorsal femoral head. The epiphyseal line at the neck is present. The area of Catterall grade 3 seems quite, but not fully included, but a good rest of grade 4 and a little bit of 3 is there like in the patient before. Pictures of the operation are not available. The last radiography, 23 years after operation (Fig. 22), shows a normal joint. Only the joint space is somewhat small.
Fig. 23 is taken from a 7 1/2 years old boy. The first picture shows a roughly folded femoral head, which still has a round outline. After the flexion osteotomy (Fig. 24) there is a dark field, which extends from the epiphyseal line up to the center line of the femoral head. The femoral neck is short.
From the straight lateral views (Fig. 25) it should have been group 2 up to the beginning of 3, but there is a rest of group 1.. The last picture however (Fig. 26) shows a very good femoral head. The femoral neck only is shortened. But the epiphyseal line is normal now and probably can produce further length.
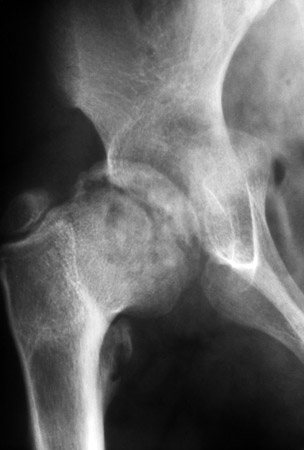
Fig. 27 of a boy, 5 1/2 years old, presents the typical picture of Catterall's group 4 at the left hip. Fig. 28 is taken orthograde laterally before operation.
The straight lateral postoperative picture (Fig. 29) shows, that in the area of group 4 and a bit of 3 there is calcification and 2 years later (Fig. 30) the femoral head is reduced and fairly covered from the acetabulum at the age of 7 1/2 years. Probably with further growth there will be more improvement.
Fig. 31 belongs to a boy about 12 years old. The radiography in neutral ap position shows the femoral head flat and dense in its bony structure. At the orthograde lateral pictures before (Fig. 32) the posterior half of the femoral head is still present. This means that Catterall groups 3 and 4 are not involved. The ap radiography postoperatively (Fig. 33) shows the femoral head round, apparently from the posterior half of the femoral head. The additional varus osteotomy was necessary.
At the lateral pictures before and after operation (Fig. 34, 35) we can discuss whether it is the Catterall group 2 or 3.
In the last picture (fig. 36) the femoral head is a flat, but completely and good covered in a good position and the epiphyseal line is present.
Judgement of the results at the measurements
Grades of Mose
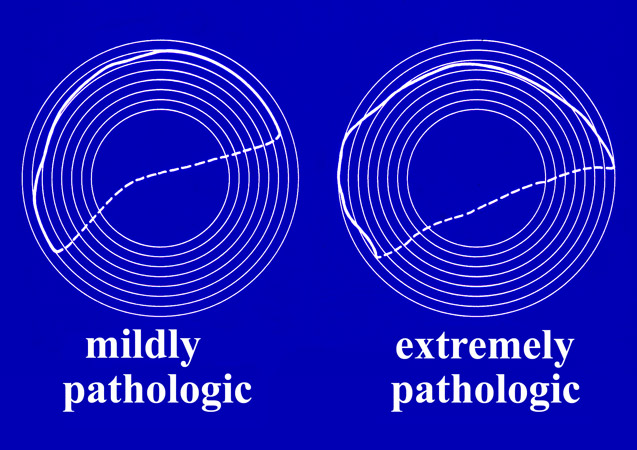
To measure the roundness of the femoral head Mose (12, 13) has introduced circles in the distance of 2 mm.
In Fig. 37 the outline of femoral heads which are not round is shown.
| Grades of Deviation for measuring to Mose | |
|---|---|
| (Tab. 1) | |
| 1 + 2 mm | Grade 1 (normal) |
| 3 + 4 mm | Grade 2 |
| 5 + 6 mm | Grade 3 |
| > 6 mm | Grade 4 |
| Mose Grade ap | pre Op (n) | post Op (n) |
|---|---|---|
| (Tab. 2) | ||
| Grade 1 | 2 | 17 |
| Grade 2 | 13 | 12 |
| Grade 3 | 16 | 6 |
| Grade 4 | 11 | 7 |
| Mose Grade ap | pre Op (%) | post Op (%) |
|---|---|---|
| (Tab. 3) | ||
| Grade 1 | 4.8 | 40.5 |
| Grade 2 | 30.9 | 28.5 |
| Grade 3 | 38.1 | 14.3 |
| Grade 4 | 26.2 | 16.7 |
Tab. 1 presents the normal value of 2 mm and deviations in degrees up to 4. In Tab. 2. the deviation degrees of the joints can be judged in numbers and in Tab. 3 in percent. The maximum preoperatively lies at grade 3, after operation at grade 1, then at grade 2. 69% of the children had a roundness of grade 1 and 2 postoperatively.
| Catterall groups |
Grades of Deviation | pre Op (%) | post Op (%) |
|---|---|---|---|
| (Tab. 4) | |||
| 2 (n=6) | 1 2 3 4 |
- 66.7 33.3 - |
33.3 33.3 33.3 - |
| 3 (n=21) |
1 2 3 4 |
9.5 38.1 28.6 23.8 |
52.4 28.6 9.5 9.5 |
| 4 (n=14) | 1 2 3 4 |
- 7.1 43.0 49.9 |
35.7 21.4 14.3 28.6 |
| Catterall groups | Grades of Deviation | pre Op (%) | post Op (%) |
|---|---|---|---|
| (Tab. 5) | |||
| < 6 years (n=11) |
1 2 3 4 |
- 36.4 45.4 18.2 |
54.5 9.1 27.3 9.1 |
| 6 - < 10 years (n=20) |
1 2 3 4 |
5.0 30.0 30.0 35.0 |
40.0 25.0 10.0 25.0 |
| > 10 years (n=11) |
1 2 3 4 |
9.1 27.3 45.5 18.2 |
27.3 54.5 9.1 9.1 |
In Tab. 4 we find the Mose grades of the Catterall groups 2, 3 and 4. The maximum is reached by group 3 with 81% of the Mose grades 1 and 2, 66.6% in group 2, but also 57.1% in the heavy group 4. The results of the different age groups we find in Tab. 5. The age group of 10 years and more came to grade 1 and 2 of Mose in 81.8%, the children 6-10 years old in 65%, the children less than 6 years age in 63.6%.
| ACM angle Acetabular depth |
pre Op (%) (n=41) |
post Op (%) (n=42) |
|---|---|---|
| (Tab. 6) | ||
| Grade 1 | 12.2 |
31.0 |
| Grade 2 | 46.3 |
31.0 |
| Grade 3 | 29.3 |
28.5 |
| Grade 4 | 12.2 |
9.5 |
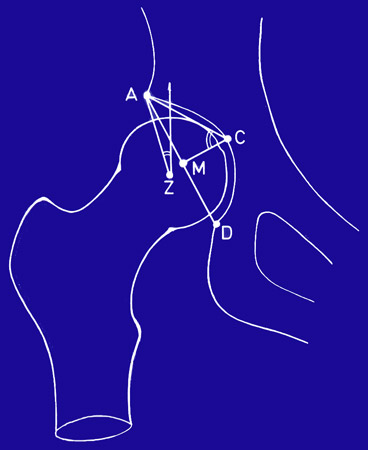
In Fig. 38 an angle - measured at C in the picture - gives a report of the depth of the acetabulum (18). It gives us the information of the pathological side of the hip. After operation the depth of the acetabulum in 62% was found at the grades 1 and 2 (Tab. 6).
| Age at Op. | Grades of Deviation | pre Op (%) | post Op (%) |
|---|---|---|---|
| (Tab. 7) | |||
| < 6 years (n=10/11) |
1 2 3 4 |
10.0 30.0 40.0 20.0 |
27.3 45.4 27.3 - |
| 6 - < 10 years (n=20/20) |
1 2 3 4 |
15.0 45.0 30.0 10.0 |
15.0 25.0 40.0 20.0 |
| > 10 years (n=11/10) |
1 2 3 4 |
9.1 63.4 27.3 - |
70.0 30.0 - - |
In this angle of the depth of the acetabulum the children older than 10 years again had the best degrees, grade 1, the normal, in 70% and grade 2, the slightly pathological in 30%, together 100%. And again the youngest group with less than 6 years followed with 72.7% and the 6 to 10 year old children with 40% (Tab. 7).
Another measurement inside the acetabulum is the breadth of the dislocation of the hip in the epiphysis (Fig. 39). Postoperatively 95.5% of the children reached the grades 1 and 2 (Tab. 8).
| Grades (mm) | pre Op (%) (n=42) |
post Op (%) (n=42) |
|---|---|---|
| (Tab. 8) | ||
0 - 10 |
40.5 |
71.4 |
11 + 12 |
33.3 |
19.1 |
> 12 |
26.2 |
9.5 |
An outside measurement is the Acetabulum-Head-Quotient of Heyman and Herndon (8) and Reimers (14) (Fig. 40). Optimal values are present between 100% and 90%, quite good between 90% and 70%, bad ones below 70%. The deviation degrees 1 and 2 were found here in 92.7% of the children (Tab. 9).
| pre Op (%) (n=41) |
post Op (%) (n=41) |
|
|---|---|---|
| (Tab. 9) | ||
Grade 1 |
26.8 |
41.5 |
Grade 2 |
63.4 |
51.2 |
Grade 3 |
9.8 |
7.3 |
The “comprehensive quotient“ of Heyman and Herndon (8) is made by adding the average measurements of Head-Neck-Quotient, Acetabulum-Quotient, Epiphysis-Quotient and Acetabulum-Head-Quotient divided by 4. But we had to drop the Head-Neck-Quotient, because it was changed by the projection of the flexion osteotomies. We then took the Joint-Surface-Quotient of Meyer (11).
| (Tab. 10) | ||
Grade 1 |
100 - 80% |
normal |
|---|---|---|
Grade 2 |
< 80 - 70% |
slightly pathological |
Grade 2 |
< 70 - 60% |
severely pathological |
Grade 4 |
< 60% |
extremely pathological |
Tab. 10 presents the normal values and the deviation degrees. 71% had reached grade 1, 19.1% grade 2, only 7.1% grade 3 and 2.4% grade 4.
Discussion and Consequences
These measured values together with our radiographies during follow-up are giving proof of the advantage of flexion osteotomies of round posterior remainders of the femoral head in Legg-Calvé-Perthes disease into a normal congruent weight bearing position, connected with normalisation of femoral anteversion. Sometimes varus or valgus osteotomies were necessary in addition.
So far children older than 10 years were not operated any more since bad results were reported (14, 17). This is converted to the opposite. They have the best results, followed by the children less than 6 years old. From 6 to 10 years the tri-radiate cartilage is growing. The growth centers at the acetabular rim are found only after 8 to 9 years of life and take part at the increased growth at puberty.
Acknowledgement
The authors wish to thank A. Catterall for his help in the preparation of this paper.
Literature
- Bauer, R., H. Jünger: Die intertrochantäre Varisierungsosteotomie zur Behandlung des M. Perthes. Arch. Orthop. Unfall-Chir. 79 (1974)187-204.
- Brüning, K., Heinecke, A., Tönnis, D.: Langzeitergebnisse der Azetabuloplastik. Z. Orthop. (1988) 266-273
- Catterall, A.: The natural history of Perthes disease. J. Bone Jt. Surg. (Br) (1971) 53: 37-53.
- Catterall, A.: Legg-Calvé- Perthes disease. Livingstone, London, 1982.
- Crock, H.V.: An atlas of the aterial supply of the head and neck of the femur in man (1980), Clin. Orthop. 152: 17-27
- Dahmen,G., Hinzmann,J.: Röntgenologischer Verlauf der Perthesschen Erkrankung. Z. Orthop.122:692.699
- Dunn, P. M.: Anteversion of the neck of the femur. A method of measurement. J. Bone Surg. (Br) (1952) 34: 181-186.
- Heymen, C, H., C. H. Herndon : Legg-Perthes disease. A method for the measurement of the roentgenograpic results. J. Bone Jt. Surg. (Am) 32 (1950) 767-778.
- Idelberger, K., A. Frank: Über eine neue Methode zur Bestimmung des Pfannendachwinkels bei Jugendlichen und Erwachsenen. Z.Orthop. 82 (1952) 571-577.
- Imhäuser, G.: Irrtümer in der Beurteilung kindlicher Hüftgelenke durch die konventionelle Röntgentechnik. Z. Orthop. (1982) 120: 93-99
- Meyer, J.: Treatment of Legg–Calvé-Perthes disease. Acta Orthop Scand (Suppl) (1964) 34:183
- Mose, K.: Legg-Calvé-Perthes disease, a comparison among three methods of conservative treatment. Universitetsforlaget, Aarhus, 1964.
- Mose, K.: Methods of measuring in Legg-Calve- Perthes disease with special regard to the prognosis. Clin. Orthop. 150 (1980) 103-109.
- Reimers, J.: The stability of the hip in children. Acta Orthop Scand (Suppl) (1980)184.
- Rippstein, J.: Zur Bestimmung der Anteversion des Schenkelhalses mittels zweier Röntgenaufnahmen. Z. Orthop. (1955) 86: 345-360
- Salter, R. B.: The scientific basis for innominate osteotomy in the treatment of Legg-Perthes disease. Clin. Orthop. (1973) 137: 2-14.
- Schulitz, K. P., H. O. Dustmann: Morbus Perthes, Spinger Verlag, Berlin, Heidelberg, New York, 1991
- Soeur, R., de Racker, C.: L'aspect anatomopathologique de l'ostéochondrite et les théories pathogéniques qui s'y rapportent. Acta Orthop. Belg. (1952),18: 57-102.
- Tönnis, D.: Die angeborene Hüftdysplasie und Hüfluxation im Kindes- und Erwachsenenalter. Springer Verlag, Berlin, Heidelberg, New York 1984.
- Tönnis,D.: Congenital Dysplasia and Dislocation of the Hip in Children and Adults, Springer Verlag, Berlin, Heidelberg, New York 1987.
- Tönnis, D. (Hrsg.): Die operative Behandlung der Hüftdysplasie. 2. Sammelstatistik des Arbeitskreises für Hüftdysplasie der DGOT. Bücherei des Orthopäden Bd. 44, Enke Verlag, Stuttgart 1985.
- Tönnis, D., Brüning, K., Heinecke, A.: Lateral Acetabular Osteotomy. Journal of Paediatric Orhopaedics Part B (1994) 3:40-46.
- Tönnis, D., Heinecke, A.: Verringerte Pfannenanteversion und Schenkelhals-antetorsion verursachen Schmerz und Arthrose. Teil 1: Statistik und klinische Folgen. Z.Orthop. (1999) 137:1153-159. Teil 2: Ätiologie, Diagnostik und Therapie. Z.Orthop. (1999) 137:160-167.
- Tönnis, D., Heinecke, A.: Current Concepts Review : Acetabular and Femoral Anteversion: Relationship with Osteoarthritis of the Hip. J. Bone Joint Surgery (Am), (1999) 81-A, NO 12.
| Download | |
|---|---|
| Flexion Osteotomies of the Fermoral Neck to bring round posterior remainders of the femoral head in Legg-Calvé-Perthes Disease into the weightbearing position - A New Technique | PDF (528 KB) |