Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Indication and Techniques of Acetabuloplasties
© Prof. Dr. med. Dietrich Tönnis
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
Introduction and Indications
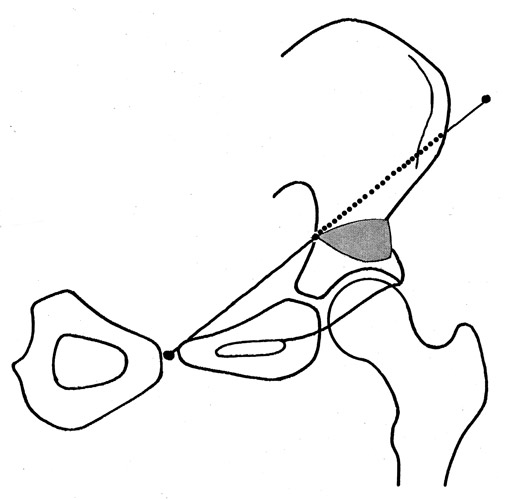
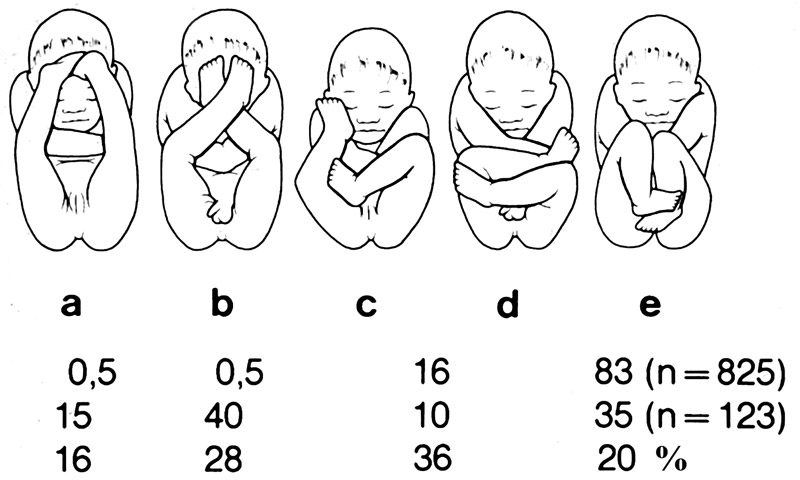 Acetabular dysplasia is developing in the fetal hip joint when the femoral head is pushed laterally or dorsally by pathological positions of the legs (Fig. 1).
Acetabular dysplasia is developing in the fetal hip joint when the femoral head is pushed laterally or dorsally by pathological positions of the legs (Fig. 1).

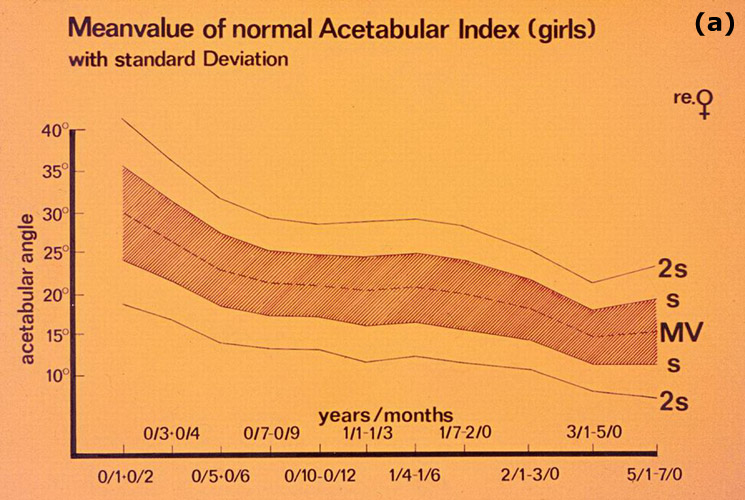
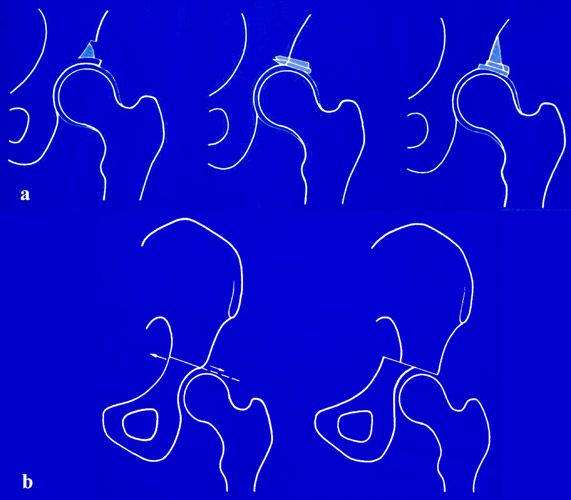
Then the capsule and the labrum are distended and elongated (Fig. 2). By this displacement, the femoral head deforms the lateral and dorsal rim of the acetabulum. After birth the joint is unstable and the femoral head dislocates even more.
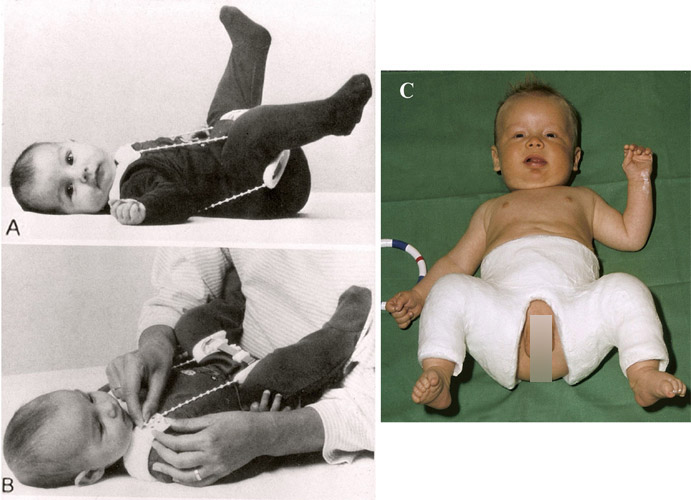 If the joint is immediately centered and sufficiently fixed, stability returns and normal acetabular growth is seen. But frequently the fixation is insufficient. A flexion-abduction splint is sufficient only in Grafs type 2 hips (Fig. 3 a, b). In the dislocated types 3 and 4 a plaster cast in the socalled human or squatting position is most effective (Fig. 3c). In the first year of life, even after open reduction, the joint will normalize spontaneously in the plaster cast.
If the joint is immediately centered and sufficiently fixed, stability returns and normal acetabular growth is seen. But frequently the fixation is insufficient. A flexion-abduction splint is sufficient only in Grafs type 2 hips (Fig. 3 a, b). In the dislocated types 3 and 4 a plaster cast in the socalled human or squatting position is most effective (Fig. 3c). In the first year of life, even after open reduction, the joint will normalize spontaneously in the plaster cast.
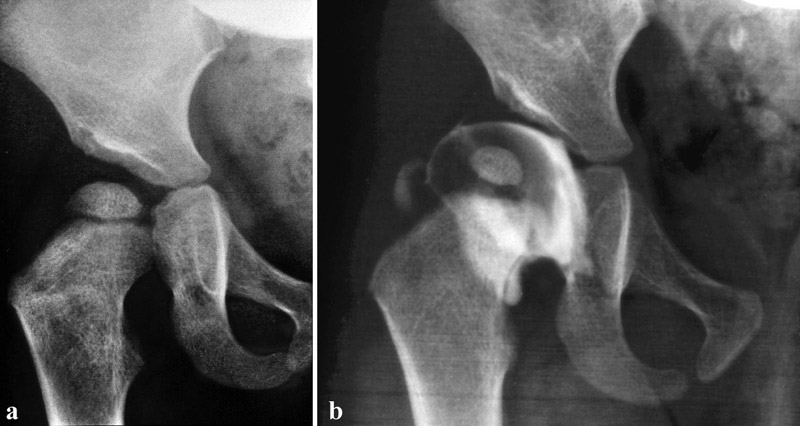
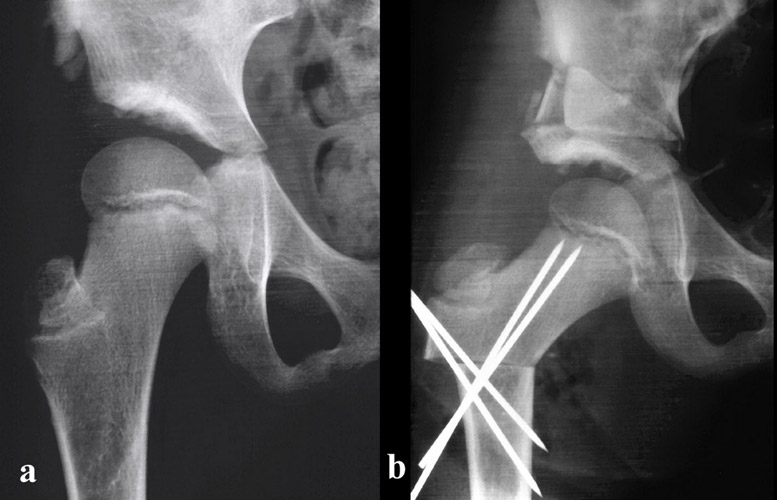
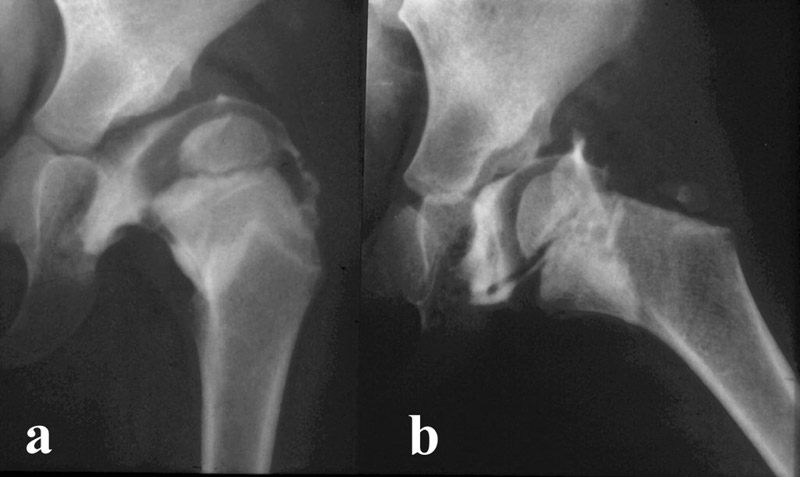
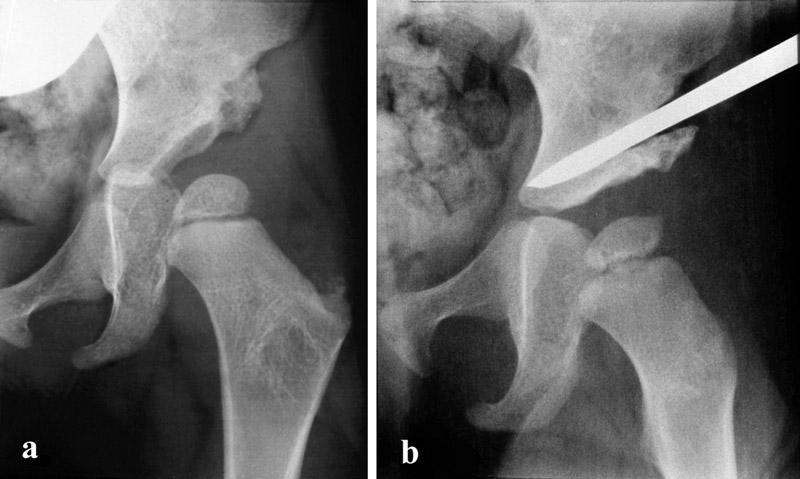
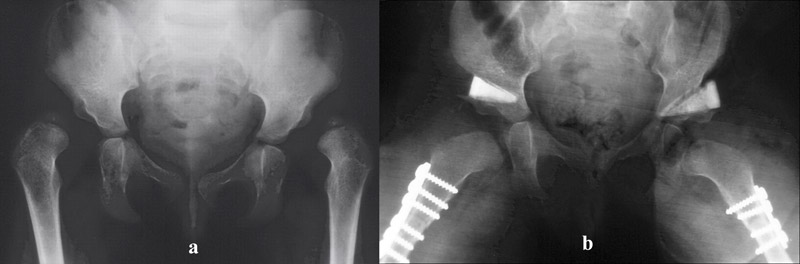
 A high dislocation of both hips is seen in Fig. 4a and reduced in Fig. 4b, but a severe dysplasia remains at both hips. Only in the first year of life a spontaneous improvement can be expected in the plaster cast. In the second year and later an acetabuloplasty is indicated immediately.
A high dislocation of both hips is seen in Fig. 4a and reduced in Fig. 4b, but a severe dysplasia remains at both hips. Only in the first year of life a spontaneous improvement can be expected in the plaster cast. In the second year and later an acetabuloplasty is indicated immediately.
Instability of the Hip
A spontaneous healing is only found in stable joints, not in the unstable (Fig. 5a). Instability is proven by palpation and by arthrography. In figure 5b instability is demonstrated by the filling of dye medially of the femoral head. In a flexed and abducted position in Fig. 5c we were able to push the femoral head out of the acetabulum, as we see by the dye filling it now. In Fig. 5d complete reduction by a central pressure was possible. This is an unstable joint. It needs a plaster cast at an age up to one year. In older children, only an acetabuloplasty can stabilize the joint.
 Acetabuloplasties are indicated only in joints that are deeply reduced by abduction. If the acetabular cavity is still filled or narrow, traction or open reduction has to be performed before.
Acetabuloplasties are indicated only in joints that are deeply reduced by abduction. If the acetabular cavity is still filled or narrow, traction or open reduction has to be performed before.
In Fig. 6b the transverse ligament of the acetabulum is narrowing the acetabular inlet. This is an example.
 When we look at Fig. 7b, the question comes up: will the left hip develop normally by itself or not. The acetabular roof is somewhat steeper than the right roof and the femoral head a bit less covered. Arthrography (Fig. 7b) shows that this is an unstable joint and this will not improve spontaneously.
When we look at Fig. 7b, the question comes up: will the left hip develop normally by itself or not. The acetabular roof is somewhat steeper than the right roof and the femoral head a bit less covered. Arthrography (Fig. 7b) shows that this is an unstable joint and this will not improve spontaneously.
Instability of the Hip
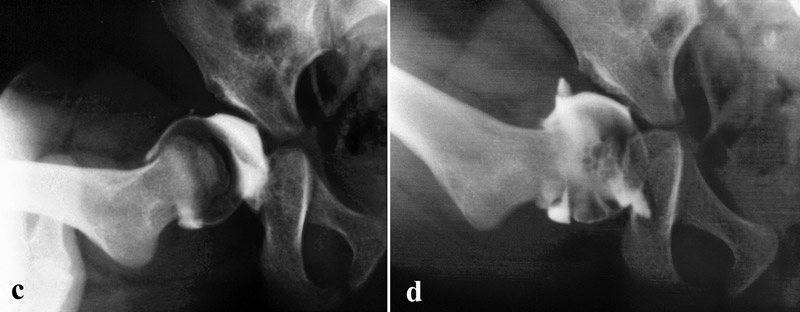
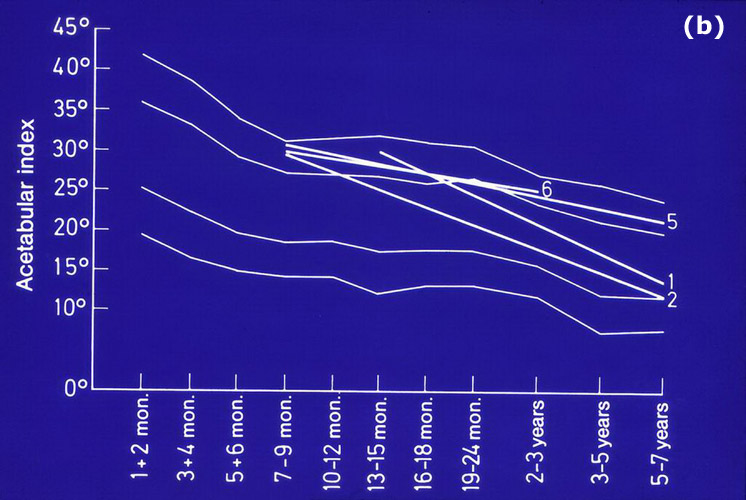
The indication for operation and for taking off the plaster cast is also based on normal values of the acetabulum. The inclination of the acetabular roof is measured by the acetabular index (AC-angle). We have evaluated normal values and borderline angles by reinvestigation (Fig. 8a). Joints between 1 and 2 standard deviations have deteriorated in 20% to pathological joints beyond 2 sd, 40% turned to normal values below 1sd and 40% stayed between 1 and 2 sd (Fig. 8b).
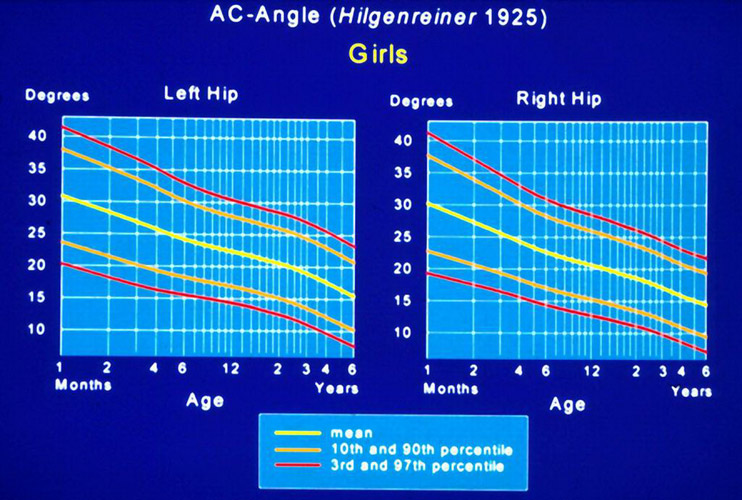 Together with Neidel percentil graphics were published for practical use (Fig. 9). Furtheron a score of normal values and degrees of deviation, mildly, moderately and severely pathological degrees, was introduced (Tab. 1). This is valuable for evaluations before and after treatment.
Together with Neidel percentil graphics were published for practical use (Fig. 9). Furtheron a score of normal values and degrees of deviation, mildly, moderately and severely pathological degrees, was introduced (Tab. 1). This is valuable for evaluations before and after treatment.
| Age (years/months) |
Normal value (mean) | Grade 1 (normal) |
Grade 2 (mildly pathological) | Grade 3 (moderately pathological) | Grade 4 (extremely pathological) |
|---|---|---|---|---|---|
0/3 + 0/4 |
25 |
< 30 |
≥ 30 - < 35 |
≥ 35 - < 40 |
≥ 40 |
0/5 - 2/0 |
20 |
< 25 |
≥ 25 - < 30 |
≥ 30 - < 35 |
≥ 35 |
2 - 3 |
18 |
< 23 |
≥ 23 - < 28 |
≥ 28 - < 33 |
≥ 33 |
3 - 7 |
15 |
< 20 |
≥ 20 - < 25 |
≥ 25 - < 30 |
≥ 30 |
7 - 14 |
10 |
< 15 |
≥ 15 - < 20 |
≥ 20 - < 25 |
≥ 25 |
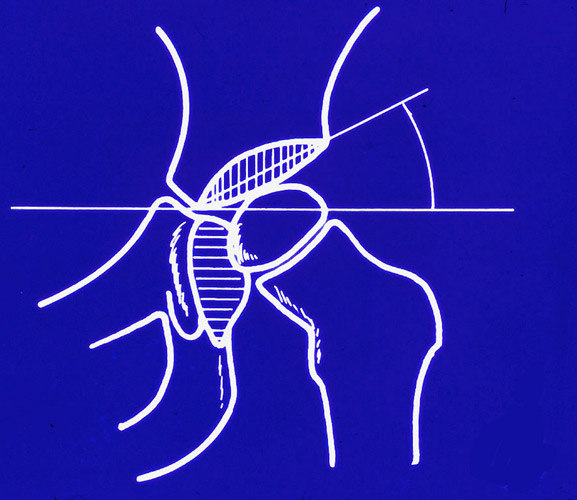 The CE- angle of Wiberg is well known. But it can be measured only after the age of 5 years. Up to 10 years the AC-angle is more significant (Fig. 10).
The CE- angle of Wiberg is well known. But it can be measured only after the age of 5 years. Up to 10 years the AC-angle is more significant (Fig. 10).
 In adolescents, after the fusion of the triradiate cartilage, the sclerotic line of the acetabular roof, the weightbearing zone after Bombelli, is the main criterion too.
In adolescents, after the fusion of the triradiate cartilage, the sclerotic line of the acetabular roof, the weightbearing zone after Bombelli, is the main criterion too.
The anterior coverage of the femoral head, the VCA angle of Lequesne and de Séze, is measured only in adolescents and adults (Fig. 11).
Different Acetabuloplasties
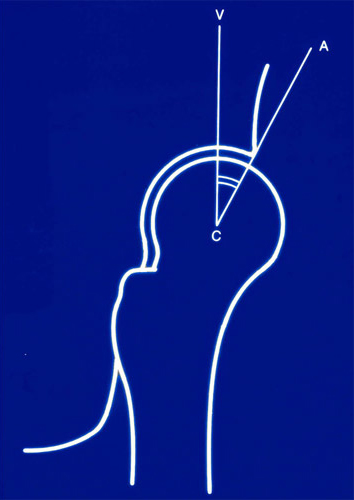
 Different procedures have been described to improve acetabular dysplasia (Fig 12a, b). The so called shelf operations at the left of König, Spitzy and others cannot be recommended any more since we have better ones. The same can be said of Chiaris osteotomy in childhood.
Different procedures have been described to improve acetabular dysplasia (Fig 12a, b). The so called shelf operations at the left of König, Spitzy and others cannot be recommended any more since we have better ones. The same can be said of Chiaris osteotomy in childhood.
 Two osteotomies are chiseling in the anterior to posterior direction, the one of Salter and that of Pemberton. Salters innominate osteotomy (Fig. 13) levers the whole acetabulum with the lower part of the pelvis in an antero-lateral direction around an axis passing through the pubic symphysis and the last posterior part of the osteotomy.
Two osteotomies are chiseling in the anterior to posterior direction, the one of Salter and that of Pemberton. Salters innominate osteotomy (Fig. 13) levers the whole acetabulum with the lower part of the pelvis in an antero-lateral direction around an axis passing through the pubic symphysis and the last posterior part of the osteotomy.
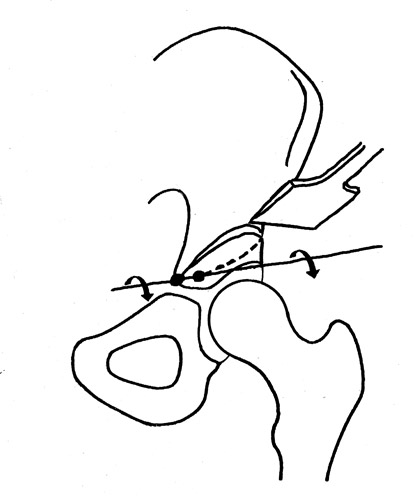 In Pembertons osteotomy (Fig. 14) the hinge for turning down the acetabular roof is the last, posterior, transverse cortical segment above the triradiate cartilage, short before the sciatic notch.
In Pembertons osteotomy (Fig. 14) the hinge for turning down the acetabular roof is the last, posterior, transverse cortical segment above the triradiate cartilage, short before the sciatic notch.
Both osteotomies, as well as the anterior rotation in the triple pelvic osteotomy, produce a retroversion or decrased anteversion of the acetabulum (Dona et al.). In the triple osteotomy we have learned that we have to rotate the acetabulum internally in addition to ventral rotation until there is a normal acetabular anteversion (15 - 20°) and a normal internal rotation of the hip (Tönnis et al.).
 Osteotomies chiseling from lateral in medial direction have been described by Albee 1915 and Jones 1920 (Fig. 15a, b). Lance propagated this technique in Europe 1925.
Osteotomies chiseling from lateral in medial direction have been described by Albee 1915 and Jones 1920 (Fig. 15a, b). Lance propagated this technique in Europe 1925.
Here the acetabular roof is partially osteotomized in a thickness of 5 - 7 mm. Only the lateral part of the acetabulum is brought into the horizontal position.
 Wiberg, in a publication 1939, had used this technique, but in 1953 he presented in Fig. 16 at the left, what Dega in 1973 called a transiliac osteotomy. Before the symposium of Chapchal 1965 in Basel, Dega used a type of Colonna acetabuloplasty in open reductions after Colonna, as he said, and Chiari and Salter osteotomies in the others.
Wiberg, in a publication 1939, had used this technique, but in 1953 he presented in Fig. 16 at the left, what Dega in 1973 called a transiliac osteotomy. Before the symposium of Chapchal 1965 in Basel, Dega used a type of Colonna acetabuloplasty in open reductions after Colonna, as he said, and Chiari and Salter osteotomies in the others.
 In a paper of 1964, the drawing of him in Fig. 17 looks like Wibergs transiliac osteotomy. But the osteotomy is performed round, not flat, and only above and around the acetabular roof, not anteriorly, and posteriorly not up to the sciatic notch. In 1973 he stated that his transiliac osteotomy does not necessarily have to reach the sciatic notch. This is different then from Wiberg and what we perform today.
In a paper of 1964, the drawing of him in Fig. 17 looks like Wibergs transiliac osteotomy. But the osteotomy is performed round, not flat, and only above and around the acetabular roof, not anteriorly, and posteriorly not up to the sciatic notch. In 1973 he stated that his transiliac osteotomy does not necessarily have to reach the sciatic notch. This is different then from Wiberg and what we perform today.
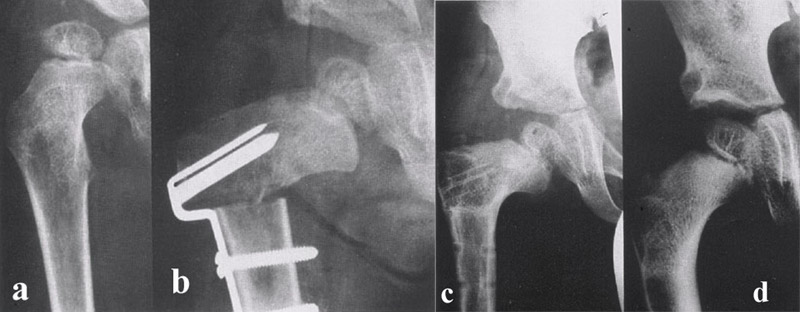
In my training in Berlin with Prof. Witt between 1960 and 1968 (Fig. 18a, b, c, d) we started also with a complete transiliac osteotomy and worked on it furtheron in Dortmund (Fig. 19a, b).
Own technique of acetabuloplasty
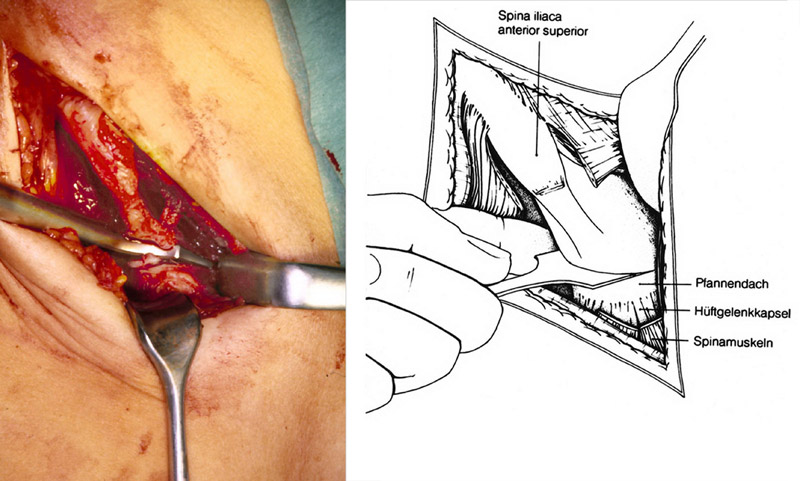 The inguinal incision is our preferred approach for open reductions and the transiliac osteotomy (Fig. 20 a, b). The scars are almost invisible. The incision starts from the anterior iliac crest to the groin parallel to the inguinal ligament. Only the most anterior part of the gluteus medius muscle is detached from the iliac crest for a length of about 3 - 4 cm, together with the tensor faciae latae and sartorius.The muscles are carefully stripped subperiostially with a wide elevator down to the joint capsule and the lateral insertion of the rectus tendon muscle. This region should not be traumatized since the growth centers of the acetabular rim are closely underneath here.
The inguinal incision is our preferred approach for open reductions and the transiliac osteotomy (Fig. 20 a, b). The scars are almost invisible. The incision starts from the anterior iliac crest to the groin parallel to the inguinal ligament. Only the most anterior part of the gluteus medius muscle is detached from the iliac crest for a length of about 3 - 4 cm, together with the tensor faciae latae and sartorius.The muscles are carefully stripped subperiostially with a wide elevator down to the joint capsule and the lateral insertion of the rectus tendon muscle. This region should not be traumatized since the growth centers of the acetabular rim are closely underneath here.
The inguinal ligament, abdominal muscles and the iliacus muscle are also detached at the iliac crest, so that we are able to palpate and see the blade of the osteotome anteriorly as it enters the inner side of the pelvis.
Then the glutaeus muscles above the capsule are stripped subperiostially back, up to the greater sciatic notch, until a finger can control the osteotomy. The gluteus muscles should be retracted gently and by rounded retractors. The superior gluteal nerve is close underneath this surface. A lesion causes limping.
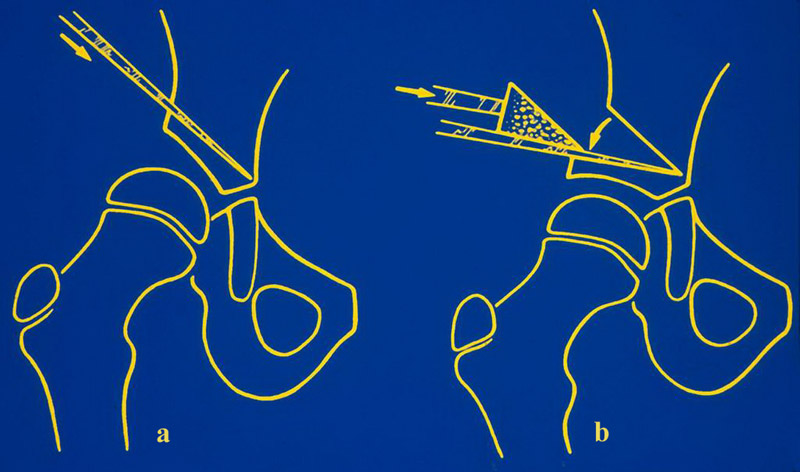
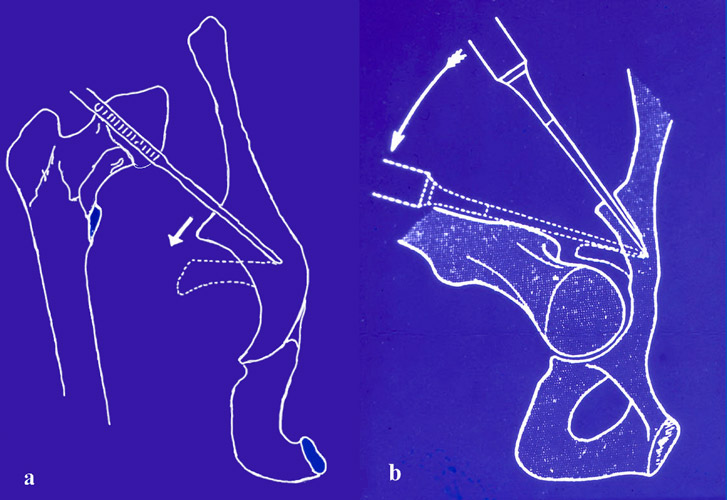
 We osteotomize the acetabular roof 6 - 8 mm above the lateral acetabular margin using a flat Lexer osteotome (Fig. 21 a, b). The operation is performed on a radiolucent table. Using an image intensifier, the blade of the osteotome is driven towards the posterior rim of the triradiate cartilage. It should stop about 4 mm before it. Anteriorly the blade passes through the anterior inferior iliac spine. Posteriorly it just enters the sciatic notch. There we check the blade position by palpation. The bone must be cut completely through from its anterior side back into the sciatic notch.
We osteotomize the acetabular roof 6 - 8 mm above the lateral acetabular margin using a flat Lexer osteotome (Fig. 21 a, b). The operation is performed on a radiolucent table. Using an image intensifier, the blade of the osteotome is driven towards the posterior rim of the triradiate cartilage. It should stop about 4 mm before it. Anteriorly the blade passes through the anterior inferior iliac spine. Posteriorly it just enters the sciatic notch. There we check the blade position by palpation. The bone must be cut completely through from its anterior side back into the sciatic notch.
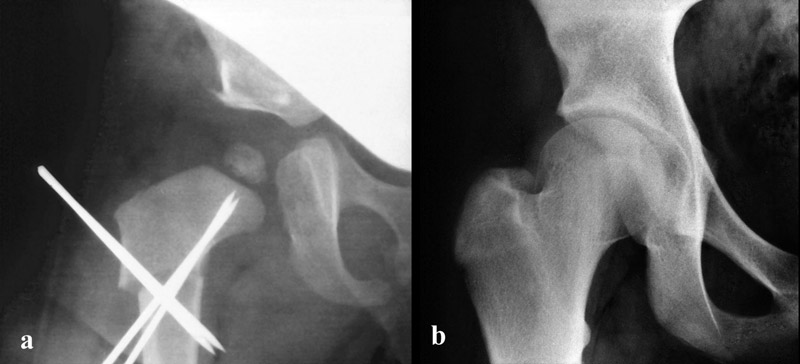
 Then a maximum turn-down of the acetabular roof is possible (Fig. 21c). The hinge is placed by the 2 cm broad blade of the chisel parallel to the posterior triradiate cartilage, at the medial side of the pelvic wing. The acetabular roof is turned down in the few millimeters of bone and the triradiate cartilage next to it posteriorly. An angle of 5-10° should be achieved. Fig. 21d, 7 years later, shows a perfect joint and coverage.
Then a maximum turn-down of the acetabular roof is possible (Fig. 21c). The hinge is placed by the 2 cm broad blade of the chisel parallel to the posterior triradiate cartilage, at the medial side of the pelvic wing. The acetabular roof is turned down in the few millimeters of bone and the triradiate cartilage next to it posteriorly. An angle of 5-10° should be achieved. Fig. 21d, 7 years later, shows a perfect joint and coverage.
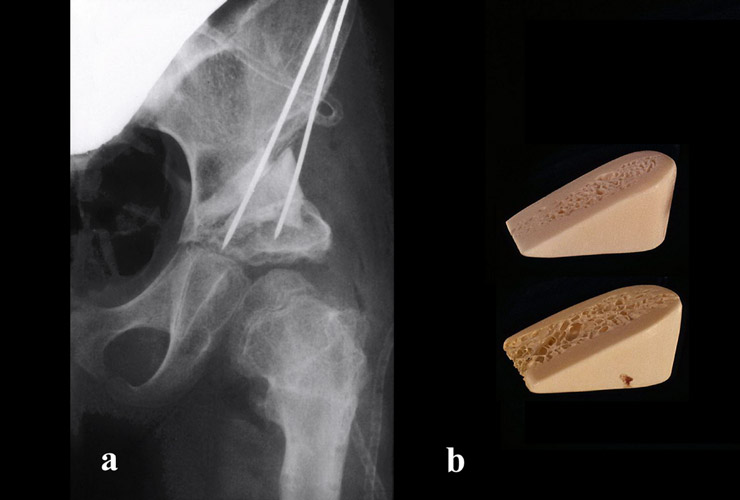
 Our maximal angles of correction have been 50° (Fig. 22a, b). This cannot be achieved by Salters osteotomy or the incomplete osteotomy of Albee, Jones and Lance. A bone wedge of an adequate height laterally is prepared then and implanted, sometimes fixed with a K-wire. Here a wedge from the bone bank has been pushed in medially and a peace of bone from the shortening osteotomy laterally. A hip spica in slight flexion of about 25° relieves the pressure on the femoral head.
Our maximal angles of correction have been 50° (Fig. 22a, b). This cannot be achieved by Salters osteotomy or the incomplete osteotomy of Albee, Jones and Lance. A bone wedge of an adequate height laterally is prepared then and implanted, sometimes fixed with a K-wire. Here a wedge from the bone bank has been pushed in medially and a peace of bone from the shortening osteotomy laterally. A hip spica in slight flexion of about 25° relieves the pressure on the femoral head.
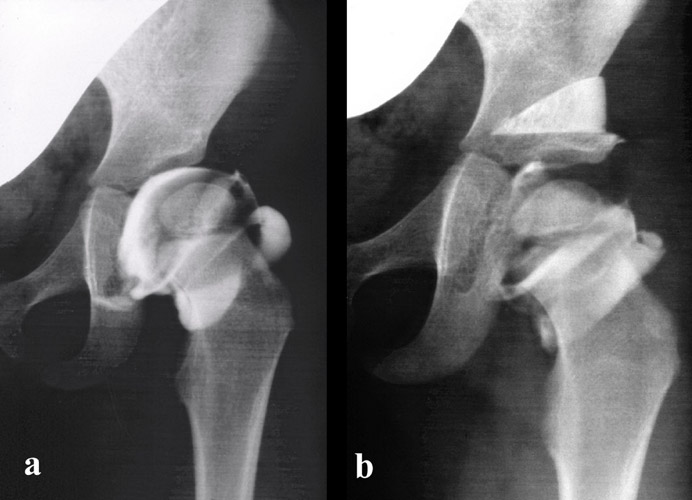
 When acetabuloplasty is combined with an open reduction and the dislocation was high (Fig. 23a, b), a shortening osteotomy is added to avoid ischemic necrosis of the femoral head.
When acetabuloplasty is combined with an open reduction and the dislocation was high (Fig. 23a, b), a shortening osteotomy is added to avoid ischemic necrosis of the femoral head.
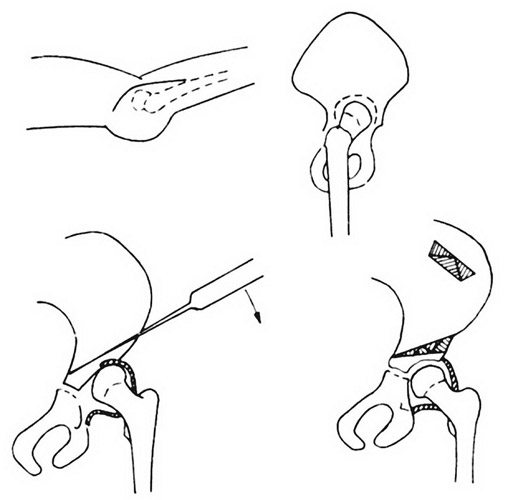
Acetabuloplasties with simultaneous varus osteotomies
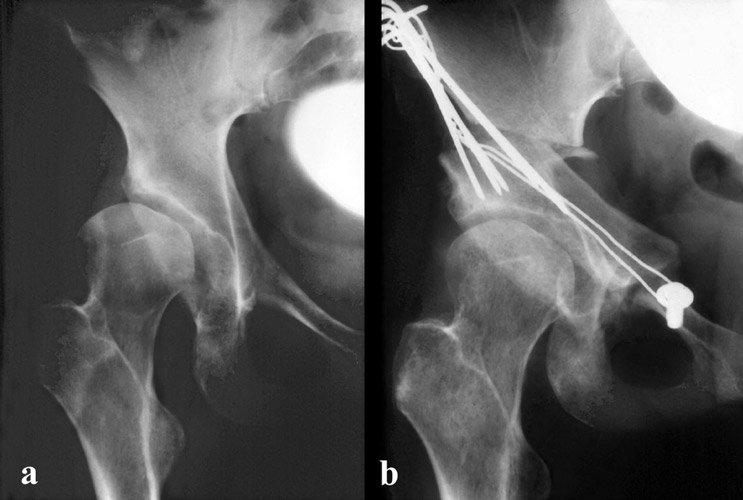
During my training in Berlin, Witt and Mittelmeier proposed a combination of acetabuloplasty with a varus osteotomy (Fig. 24a, b). The bone wedge from the osteotomy was placed above the osteotomized acetabular roof. Later we used deproteinized bone wedges from animals produced by Braun/Melsungen (Fig. 25a, b). The lateral wall of the wedge had to be firm, the inside spongious. The wedges were replaced by own bonegrowth in a few years and worked very well.
 But later this was not allowed any more. Then we used bone wedges prepared from human femoral heads of the bone bank (Fig. 26).
But later this was not allowed any more. Then we used bone wedges prepared from human femoral heads of the bone bank (Fig. 26).
The wedges are sterilized at 121° C for 20 minutes and then kept deep-frozen in the bobank. M. Ekkernkamp and Katthagen have reinvestigated 121 joints. All had best results.
 The hip spica we leave for 6 weeks. Only in open reductions we have to decide whether stability of the joint is already sufficient. It is the advantage of this acetabuloplasty, that the stability is immediately increased.
The hip spica we leave for 6 weeks. Only in open reductions we have to decide whether stability of the joint is already sufficient. It is the advantage of this acetabuloplasty, that the stability is immediately increased.
We can see it in Fig. 27b how the femoral head is shifted more medially and distally after acetabuloplasty. The dye has left the joint and the upper labrum has come down far laterally, embracing and holding the femoral head.
Comparison with other techniques
This is not achieved in Salters osteotomy (Fig. 13) and it takes a longer time until the joint and the lower pelvic part has normalized after the extreme inclination that was given. Also a number of dorsal redislocations were observed in America. And we mentioned already the problembs of retroversion resulting from the anterior rotation. In small children this maybe changed during growth, but in the elder ones probably not.
In Pembertons osteotomies (Fig. 14) the results look similar to ours since it is also a full transiliac osteotomy, only from another direction. A disadvantage of this operation during chiseling is only that you cannot use the image intensifier in a normal position. You have to rotate the pelvis to observe the motion of the blade. Then the osteotomy cannot be as exactly. A decrease of acetabular anteversion is certainly present, but not as much as in Salters osteotomy.
First Long-Time Follow-Up
In a first long-time follow-up of children with additional varus osteotomies in 1988 we reviewed 90 hip joints in 67 children (Brüning et al.). The age at operation was in average 3.6 years, the age at follow-up 15 years. The clinical results are shown in Tab. 2. They are perfect. Only the Trendelenburg limp was relatively high in grade 3 with 13.5%. Therefore we advise to be very careful laterally at the muscles and the nerve at the acetabular rim.
But we have to consider the frequency of previous operations in other hospitals (Tab. 3). 29% of the children had preoperatively an avascular necrosis of the femoral head after treatment with a plastercast in Lorenz position. Finally the number of concomitant operations at acetabuloplasty was high (Tab. 4).
No pain or only occasional |
98% |
|
No limitation of movement |
||
Trendelenburg limp negativ |
71% |
|
| Grade 1 | 15.5% | |
| Grade 3 | 13.5% | |
Open reductions |
22% |
Femoral osteotomies |
10% |
Other acetabular operations |
5.6% |
Acetabuloplasty and Varus Osteotomy |
64.4% |
Acetabuloplasty and Varus Osteotomy after earlier Open Reduction |
24.4% |
Acetabuloplasty with concomitant Open Reduction |
6.7% |
Acetabuloplasty with concomitant Open Reduction and Varus Osteotomy |
2.2% |
Acetabuloplasty alone or with shortening osteotomy |
2.2% |
The mean values of the joints are shown in Tab. 5. They are all normal for that age. When we investigated the score of normal values and deviation degrees, which we mentioned in the beginning, we found for the different measurements percentages of normal and slightly pathological values mainly between 62% and 93% (Tab. 6).
CE angle |
26° |
Weight bearing zone angle |
9.7° |
Migration percentage |
12.3% |
Distance to teardrop |
8.8 mm |
Acetabular angle (Ullmann, Sharp) |
93.2% |
Acetabular angle (Weight bearing zone) |
62.0% |
CE angle (Wiberg) |
82.0% |
Migration percentage (Reimers) |
91.0% |
Distance femoral head - teardrop figure |
87.6% |
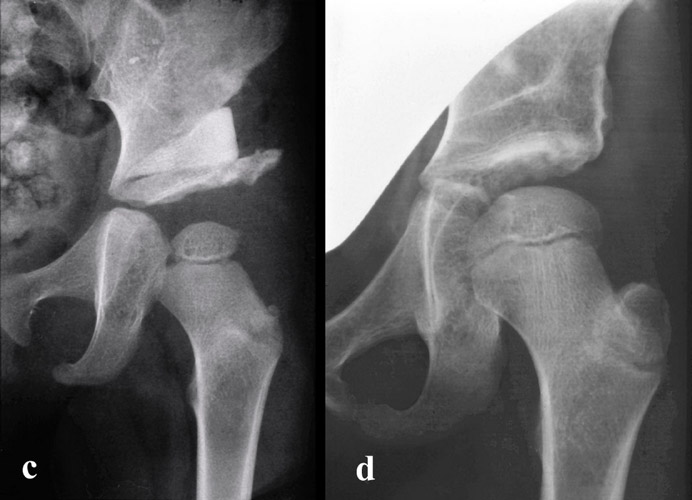
Critical were only two measurements of the femoral neck, the epiphyseal index and the head-neck index. They presented only 50% of normal and slightly pathological values (Tab. 7). These patients had a tilt of the femoral head, a socalled head-in-neck position or subcapital coxa valga after varus osteotomy (Fig. 28a, b). Ever since we avoided varus osteotomies.
Neck-shaft angle |
86.7% |
Antetorsion angle |
74.5% |
Epiphyseal index (Eyre-Brook) |
50.0% |
Head-neck index (Heyman-Herndon) |
47.7% |
Epiphyseal KE angle |
76.5% |
Last Reinvestigation
A recent reinvestigation of acetabuloplasties without varus osteotomy and with sterilized and deep frozen bone wedges in 52 hips has been performed beween 2 months and 9 years after operation by Bonmann. The femoral neck showed a normal development now in all joints.
The material consisted of 158 children operated between 1.1.91 and 31.12.92, reinvestigated late in the year 2000, so follow-up 8-10 years. Age at operation 3.1 years, at follow-up 12.0 years. Patients with previous or additionsl operations like open reductions and femur osteotomies or neurologic diseases were excluded. The material then consisted of 83 children with 125 operated joints. 91.2% of all patients of this type were investigated.
| Angle | Before operation | At follow-up | Valuation |
|---|---|---|---|
| AC anle | 30° | 9.6° | normal |
| CE angle | 5.3° | 35.3° | normal |
| Ullmann-Sharp angle | 73 hips normal, 9 slightly pathological | ||
| Harris hip score | 75 very good, 8 good | ||
| Patients' opinion | 96.4% good and very good, one not |
In Tab. 8 the results are presented. The AC angle was corrected from 30° to 9.6°, a normal angle, the CE angle from 5.3° to 35.3°, very good, Ullmann-Sharps angle in 73 hips normal, in 9 slighly pathological. The Harris hip score was very good in 75 hips, good in 8 hips. The opinion of the patients was considered good and very good in 96.4% and not good in only one.
These results and other physical ones are as good as wanted and speak for this type of acetabuloplasty.
Conclusion
 Acetabular coverage in acetabular dysplasia is achieved to the best degree in complete transiliac osteotomies without varus osteotomies at an age up to 9 or 10 years, when the triradiate cartilage fuses, but even a few years later.
Acetabular coverage in acetabular dysplasia is achieved to the best degree in complete transiliac osteotomies without varus osteotomies at an age up to 9 or 10 years, when the triradiate cartilage fuses, but even a few years later.
Later, the whole acetabulum has to be rotated laterally and anteriorly after disconnecting it from the os pubis, os ischium and os ilium by a socalled triple pelvic osteotomy (Fig. 29). But this operation is more difficult and takes a longer time to recover. Residual dysplasias therefore should be treated as early as possible in the way demonstrated here.
| Download | |
|---|---|
| Indication and Techniques of Acetabuloplasties | PDF (2.6MB) |