Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Langzeitergebnisse nach offener Einstellung von Hüftluxationen von einem ventralen Zugang, erst lateral, dann medial des M. Iliopsoas
© Prof. Dr. med. Dietrich Tönnis, Wolfgang Cordier, M.D., Klaus Kalchschmidt, M.D., Klaus Storch, M.D., Bernd Dietrich Katthagen, M.D.
Alle im Text verwendeten Abbildungen lassen sich per Mausklick vergrößert darstellen! Am Ende des Textes finden Sie darüber hinaus ein PDF zum Download.
Einführung
Mit der heutigen Früherfassung von Hüftdysplasien und -luxationen durch das Neugeborenenscreening mit Ultraschall geht die Zahl der operativen Hüftrepositionen zurück und die Erfahrung in diesen Eingriffen verringert sich. Deshalb erscheinen Erfahrungsberichte über ein grösseres Krankengut, verschiedene Operationstechniken, und eine langfristiger Beobachtungszeit wichtig.
Unsere Klinik befasste sich ab 1970 schwerpunktmässig mit der Behandlung von Hüftdysplasien und -luxationen. Die Erfahrungen und Ergebnisse der operativen Hüftluxationseinstellung sollen deshalb hier mitgeteilt werden.
Operatives Vorgehen
Eine tiefe konzentrische Einstellung des Hüftkopfes wird oft durch mediale Anteile der Kapsel und des Labrums am Pfannenrand und durch verspringende Teile des Ligamentum transversum der Pfanne verhindert. Doese Strukturen müssen entfernt oder durchtrennt werden, bis der Hüftkopf tief an den Pfannenboden treten kann. Diese Pfannenanteile sind oft schwer zu identifizieren und von einem lateralen operativen Zugang zu erreichen. Vorsicht ist auch geboten, dass die azetabulare Arterie und Vene am Pfannenboden nicht verletzt werden.
Deshalb haben wir uns von dem antelateralen Zugang zu einem inguinalen von vorn zugewendet (Tönnis 1978). In der Leistenbeuge wird die Faszie unmittelbar unter dem Leistenband durchtrennt. Der Tensor fasciae latae und der Sartorius-Muskel werden an der Spina iliaca superior abgelöst und der M. rectus femoris an der Spina iliaca inferior und mit dem Wundrand nach medial zurückgezogen. Der vordere Rand des M. glutaeus mamimus wird an seinem Vorderrand ein kleines Stück abgelöst in seinem knorpeligen Rand. Das Leistenbandmit der abdorminalen Muskulatur werden auch am Beckenkamm abgelöst und nach cranial gezogen.
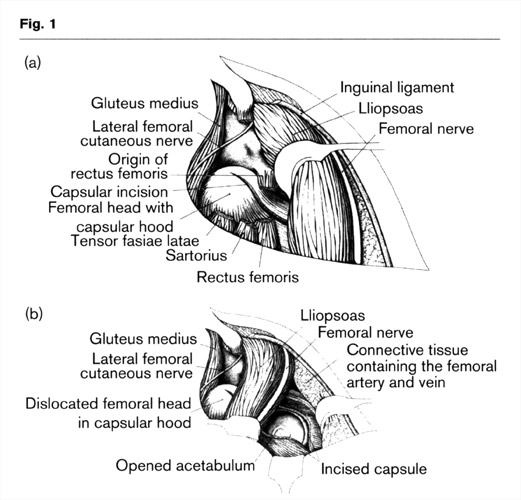 Die freigelegte Gelenkkapselwird jetzt mindestens 0,5 cm parallel zum Pfannenrand eingeschnitten unter Schonung des Labrums und der darunter liegendenen apophysialen Wachstumszentren. Jetzt wird der M. iliopsoas nach der Technik von Tönnis etwas zur Seite gezogen, so dass wir uns dem Gelenk in der Lacuna musculorum nähern können (Abb. 1a).
Die freigelegte Gelenkkapselwird jetzt mindestens 0,5 cm parallel zum Pfannenrand eingeschnitten unter Schonung des Labrums und der darunter liegendenen apophysialen Wachstumszentren. Jetzt wird der M. iliopsoas nach der Technik von Tönnis etwas zur Seite gezogen, so dass wir uns dem Gelenk in der Lacuna musculorum nähern können (Abb. 1a).
Anfangs haben wir den Nervus femoralis, der auf dem Muskel liegt, isoliert und nach lateral gezogen aber es ist schonender für den Nerv, wenn er auf dem Muskel belassen wird und mit doppelt gerundeten Wundhaken zurück gehalten wird. Die Iliopsoassehne wird ein Stück durchtrennt, um anschließend Druck durch Verlängerung und Nekrosen des Hüftkopfes zu vermeiden. Das mediale Gewebe des Lacuna vaserum mit der Arteria und Vena femoralis wird mit doppelt gerundeten Haken zurück gehalten.
Dieser Zugang gibt eine excellente Übsersicht über die Pfanne und ihre mediale Grenze. Die Tiefeinstellung des Hüftkopfes und der Pfannenrand sind exakt zu sehen (1, 2, 3). Der Zugang betrifft damit nur die Hüftpfanne und schont auch das Gefäßnetz des Schenkelhalses. Bei Verkürzungsosteotomien lässt sich auch eine subtrochantäre Osteotomie mit Anlagerung einer 4-Lochplatte leichter als eine Varisierung durchführen. Es wird dann geprüft, ob Luxationsbereitschaft noch besteht wegen der Steilheit des Pfannendaches. Es lässt sich dann auch von hier eine Acetabularplastie (Abb. 2) durchführen.
Bei Verkürzungsosteotomien lässt sich auch eine subtrochantäre Osteotomie mit Anlagerung einer 4-Lochplatte leichter als eine Varisierung (Abb. 2a, b, c) durchführen. Es wird dann geprüft, ob Luxationsbereitschaft noch besteht wegen der Steilheit des Pfannendaches. Es lässt sich dann auch von hier eine Acetabuloplastik (Abb. 2) durchführen.
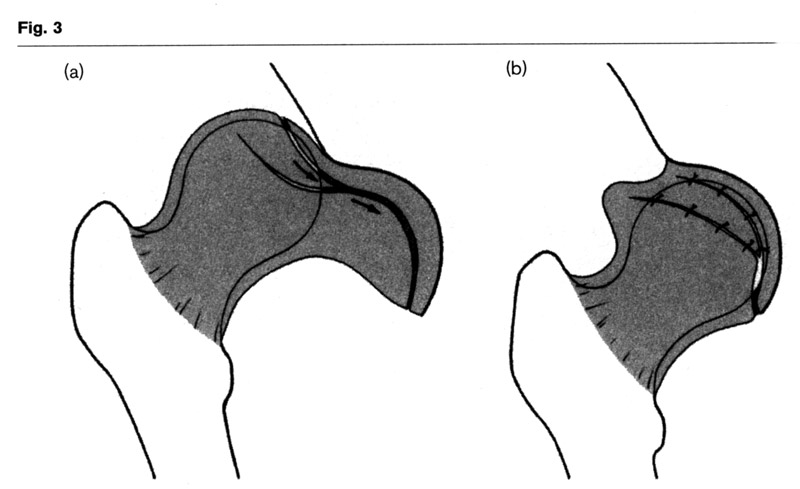 Auch eine Kapselraffung (3) kann durch einen Lappen aus der hinteren Kapsel gut durchführen. (Fig. 3 a, b).
Auch eine Kapselraffung (3) kann durch einen Lappen aus der hinteren Kapsel gut durchführen. (Fig. 3 a, b).
The flap is pulled ventrally like a girle around the femoral head narrowing the capsule dorsolaterally and widening it in the former narrow ventral part with the interposition. A plaster cast is given at least 6 weeks or longer according to the stability and the degree of residual dysplasia.
Krankengut
Für die Auswertung der operativen Hüfteinstellung wurden nur Kinder einbezogen, bei denen es sich um "typical congenital developmental disclocations" handelte, nicht um "teratological dislocations", und das Alter zwischen O und 4 Jahren lag. Revisionsoperationen von anderernorts vorbehandelten Patienten wurden nicht ausgewertet. Bei der Nachuntersuchung sollte Skelettreife vorliegen. Alle Unterlagen mussten vollständig sein.
Von 87 Patienten kamen dann 86 zur Nachuntersuchung. 70 Patienten waren weiblich, 17 männlich. Bei 31 war die Hüftluxation beidseitig. Damit konnten 117 Gelenke untersucht werden. Das Alter lag zum Zeitpunkt der Operation zwischen 3 Monaten und 4 Jahren, im Mittelwert bei 1 Jahr, 3 Monaten. Die Beobachtungszeit verteilte sich zwischen 10 und 21 Jahren und lag im Mittelwert bei 15 Jahren, 3 Monaten.
Die Schweregrade der Luxation nach Tönnis (2, 16) verteilten sich bei 117 Gelenken wie folgt:
Grad 2 (Kopfkern nur lateralisiert): 0.9%
Grad 3 (Kopfkern auf Höhe des Pfannenerkers): 17.9%
Grad 4 (Kopfkern oberhalb des Pfannenerkers): 81.2%
Die Art der Eingriffe, die bei der Operation verwandt wurden, geht aus Tab. 1 hervor.
| Operative Hüfteinstellung ausschließlich | 27,4 % |
| Operative Hüfteinstellung und Azetabuloplastik | 31,6 % |
| Operative Hüfteinstellung, Azetabuloplastik, DVO | 30,8 % |
| Operative Hüfteinstellung, Azetabuloplastik, DVO, Verkürzungsosteotomie | 2,4 % |
| Operative Hüfteinstellung, Azetabuloplastik, Verkürzungsosteotomie | 3,4 % |
| Operative Hüfteinstellung, DVO | 4,3 % |
Ergebnisse
1. Klinische Befunde
Schmerz, Hinken und Bewegungseinschränkung wurden nach einem Fragebogenschema erfasst (Tab. 2). Bei der subjektiven Gesamteinschätzung wurden von 117 Gelenken 65.8% als sehr gut eingeschätzt, 23.9% als gut, 8.6% als ausreichend und 1.7% als schlecht.
2. Röntgenologische Auswertung
Die Überdachung des operativ reponierten Hüftkopfes ohne und mit Azetabuloplastik wurde durch den seitlichen Überdachungswinkel CE nach Wiberg (17) und den vorderen Überdachungswinkel VCA nach Lequesne and de Sèze (18) beurteilt. Von diesen Autoren werden Winkel über 25° als normal angesehen. Im Mittelwert liegen die Normalwerte allerdings bei 35° im Erwachsenenalter (22), zwischen 8 und 18 Jahren bei 32° (2).
Abb. 1 und 2 zeigen, dass der weitaus überwiegende Teil der Gelenke teils durch spontane Nachreifung und teils durch Azetabuloplastik (siehe Tab.1) voll normalisiert werden konnte, der CE-Winkel in 75,2 % und der VCA-Winkel in 82,6 % auf mehr als 25°, also Normwert, in 17,1 % bzw. 4,1 % auch auf den grenzwertigen Winkel von 20-25°, so dass nur 7,7 % bzw. 13,3 % als Restdysplasien verbleiben, die noch nachzukorrigieren sind. Das darf als sehr gutes Ergebnis angesehen werden.
3. Klinische und röntgenologische Klassifikation der Ergebnisse nach Severin
Um Vergleiche mit anderen Autoren zu ermöglichen, wurden die Hüftgelenke auch nach den Bewertungschemen von Severin (17) klassifiziert. Tab. 3 A zeigt die klinischen Ergebnisse. 82,9% gehörten zur Gruppe A, die symptomfrei ist, 15.4% zur Grppe B, die nur bei grösseren Anstrengungen etwas Beschwerden hat. 1.7% fallen in die Grupen C und D, die ein Hinken oder eine Gehstreckenbegrenzung auf 4-5 km haben.
Table 5 shows the roentgenologic results: 62 % have normal hips with an CE angle according to Wiberg (17) of more than 25° which is appropriate for their age. Group 2 also comprises hips with normal angles, however, there are slight changes of the femoral head or neck or the acetabulum. These 14 % may also be considered good. Only 7 % belong to group 3 and 4 representing residual dysplasia with CE angles below 20°. Severin does not specifically consider angles between 20 - 25°. We found 20 hips in this range and assessed them separately for statistical reasons (Tab. 6).
During long-term follow-up no case of redislocation was observed (Severin group 6), however, thirteen of our hips already redislocated while still in plaster cast. They were immediately repositioned with concomitant acetabuloplasty where necessary and were reinvestigated with the other patients.
| Classification | n | % |
|---|---|---|
| Severin 1 | 73 | 62 |
| Severin 2 | 17 | 14 |
| Severin 3+4 | 8 | 7 |
| CE angle 20–25° | 20 | 17 (not classified) |
4. Outcome according to age and type of Operation
It is generally known that outcome is age-dependant. The younger the child the more spontaneous acetabular development will occur (Fig. 4). For this reason Table 6 contains one group in which only surgical reduction and no other additional procedure such as acetabuloplasty or femoral osteotomy was performed. 29 of 32 hips were operated in the first year of life alter the third month and only three in the second year. Mean age was 7 months. In the older age group with a mean age of 17 months, 86 joints were operated at the age of 2 to 4 years and only 20 in the first year of life. In 88% of those hips operated an mainly during the first year of life, a roentgenologic improvement according to Severin's group 1 Gould be achieved (healing) (Tab. 6) whereas only 71% of the hips in whom treatment started in their second to fourth year of life achieved healing, although two thirds of these hips had undergone acetabuloplasty already. Apparently, after the first year of life sufficient spontaneous improvement without additional operative Intervention can not be regularly expected.
| Age at operation | CE Severin >25° | Clinical Severin Grade A+B |
Residual dysplasia CE angle <20° |
Avascular necrosis (Hirohashi) |
|
|---|---|---|---|---|---|
Only open reduction (n = 32) |
7 months |
88% (n = 29) |
94% |
0% |
Including 6% preoperative |
With additional procedures (n = 86) |
17 months |
71% (n = 61) |
77% |
8% |
12% grade 2+3 including 6% preoperative |
5. Complications
Table 7 gives an overview of the complications we observed. Coxa magna was determined by comparing the greatest diameter of the femoral heads of both sides in the horizontal plane at neutral leg position. Gamble et al. (25) considered an increase of more than 15% as coxa magna, whereas Imatani et al. (26) used a limit of 20%. In our investigation we applied the latter value of 20%.
| Complication | n | % |
|---|---|---|
| 1 Coxa magna was evaluated only in 54 unilateral open reductions | ||
| Coxa magna1 (n=54) | ||
| Difference in head diameter 0–20% | 10 | 19 |
| Difference in head diameter >20% | 1 | 2 |
| Avascular necrosis (Hirohashi et al.) only postoperative | ||
| Grade 1 | 7 | 5.9 |
| Grade 2 | 2 | 1.7 |
| Grade 3 | 0 | 0 |
| Total | 9 | 7.6 |
| Redislocations short after open reduction | 13 | 11 |
| Superficial wound infections | 3 | 3 |
A vascular necrosis of the femoral head was assessed according to the classification of Hirohashi et al. (27). In brief, mild necrosis does not lead to permanent damage, moderate necrosis leads to partial damage and severe necrosis to complete damage. Out of 118 hips 7 (5.9%) presented postoperatively mild avascular necrosis and 2 (1.7%) partial necrosis (Grade 2), which adds up to a total of 9 (7.6%) (Tab. 7).
| Patient Number |
Pretreatment | Osseous nucleus |
Age at operation (months) |
Necrosis grade |
|
|---|---|---|---|---|---|
| + moderate; ++ extensive | |||||
1 |
++ |
No |
13 |
3 |
|
2 |
++ |
No |
0 |
3 |
|
3 |
+ |
No |
18 |
3 |
|
4 |
+ |
Small |
17 |
1 |
|
5 |
++ |
Necrosis |
14 |
3 |
|
However, 5 (4.2 %) other hips showed already preoperatively corresponding signs after a failing longer conservative treatment.
In one femoral head a necrosis was seen, in the others no ossific nucleus and a small one in one hip.
All these hips except one were operated in the second year (Tab. 8). The missing nucleus at that time is a sign of preoperative necrosis.
The surgical technique of shortening osteotomy, often combined with acetabuloplasty, was additionally examined (Tab. 7). This procedure decreases the pressure exerted an the femoral head after reduction from the high dislocation position and an additional levering down of he acetabular roof. In this group no necrosis was observed although the age at operation was averaging 26 months. These children were definitely older than the rest of our patients (average age at operation of 17 months) and shortening osteotomy was performed in grade 4 dislocations only. 6 joints of the first group with shortening osteotomies had an age of one year to one year and six months. The joints of 4 children were operated at the age of two years, four months, to four years, four months.
In 13 hips (11%) redislocation occurred while still in plaster cast. These hips were immediately reoperated. As a result, acetabuloplasty at the time of open reduction was performed more and more often, whereas varus and detorsion osteotomies were given up almost completely (see chapter of indication in the beginning). Neither joint nor deep wound infections were observed. Only in 4% superficial infection occurred.
Discussion
| Age at operation | Shortening | Degree of dislocation | Avascular necrosis | ||
|---|---|---|---|---|---|
| See groups in Table 3 | |||||
Reduction + shortening (n = 10) |
26 months |
2 cm |
All degree 4 |
None |
|
Other reductions (n = 108) |
17 months |
None |
Degree 4, 83% |
1.8 % |
|
Degree 3, 3% including 4.2% preoperative |
|||||
When we compare our results 76 % of Severin grades 1 and 2 for the x-rays and 98 % for the Severin clinical grades A and B with other authors, that have follow-up times of 10 years and more in Table 9, we find us in the group of the four best results of 75 % and more for grades 1 and 2 of the x-rays.
The clinical grades unfortunately were investigated only rarely by other authors.
88% of the children who had undergone open reduction mainly within their first year of life achieved grade 1 of the roentgenologic classification of Severin (normal) compared to only 71% of children operated an mainly in the second to fourth year of life (Tab. 6). For the clinical classification of Severin 83% of the cases in both groups reached the standard grade of group A. Considering group A and B as well as 1 and 2 according to Severin together, the values are 98% and 76%, respectively.
Our patients presented with 5.9% grade 1 and 1.7% grade 2% a very low and mild rate of postoperative avasccular necroses when we compare in Table 10 the rate of other approaches to the hip joint. This is certainly due to our anterior approach medial to the iliopsoas muscle which is not touching the vessels of the femoral neck. No necrosis was seen after shortening osteotomies (n=10) (Tab. 9). Since then for all dislocations of higher degrees, reduction was performed sirnultaneously with a subtrochanteric osteotomy (Fig. 2a). The subtrochanteric technique was chosen to avoid damage to the proximal femoral vessels. Additionally, in a child of up to two or three years it is easier to perform a subtrochanteric than an intertrochanteric osteotomy.
| Study | Age (months) | Mean follow-up (years) | Number of hips | Avascular necrosis (%) | Redislocations (%) | Severin radiograph | Severin clinical | Operative technique | |
|---|---|---|---|---|---|---|---|---|---|
| DVO: detorsion-varus osteotomy | |||||||||
| Mean | Range | ||||||||
Berkeley [28] |
ND |
12–36 |
6.1 |
5.1 |
ND |
ND |
92 grade I+II |
100 grade A+B |
Iliofemoral approach, acetabuloplasty |
Powell et al. [29] |
16 |
4–26 |
4.3 |
16 |
25 grade I+II Salter, Gage, Winter |
ND |
68.8 grade I different score |
ND |
Anterior approach |
27 |
8–80 |
4.8 |
18 |
22.3 grade II+IV |
5.6 |
2.2 grade I different score |
ND |
Anterior approach + varus osteotomy |
|
29 |
15–46 |
5.6 |
15 |
46.7 grade I–IV |
26.7 |
46.7 grade I different score |
ND |
Anterior approach, varus + Salter osteotomy |
|
Galpin and Wenger [30] |
>2 |
ND |
3.7 |
33 |
9.1 |
12.1 |
72.7 |
ND |
Medial approach, Salter osteotomy |
Williamson [24] |
4.3 |
3–9.5 |
16.7 |
45 |
13.3 |
ND |
51 grade I+II |
80 grade A+B |
Anterior approach of Sommerville |
Castillo [31] |
19 |
5–26 |
7 |
26 |
15 |
12 |
73 grade I+II modified |
ND |
Ludloff |
Dhar [32] |
Different groups |
ND |
5.6 |
99 |
23.2 |
4 |
75.8 grade I+II |
100 MacKay grade I+II |
Anterior approach derotation |
Mergen [33] |
12.1 |
3–33 |
7.1 |
31 |
9.7 |
0 |
67.7 grade I+II |
100 MacKay grade I+II |
Medial approach (Ferguson) |
Mankey, Staheli [34] |
12 |
2–63 |
6 |
66 |
11 |
4.6 |
In 33% pelvic osteotomy later |
Ludloff |
|
Sugimoto et al. [35] |
<84 |
ND |
>15 |
43 |
46.5 Kalamchi I+II |
ND |
41.2 grades I,II,III |
ND |
Unknown |
Doudoulakis, Cavadis [36] |
7 |
2–12 |
13 |
69 |
13 |
1.5 |
76.8 successful |
Anterior approach (Smith-Petersen) |
|
Gulman et al. [37] |
ND |
19.2–48 |
13 |
43 |
34 grade II, III, IV |
71.1 |
78.9 grade I+II |
ND |
Anterior approach |
Michiels [38] |
8.8 |
3–21 |
11 |
21 |
38 |
0 |
81 grade I+II |
47.6 different score |
Ludloff and others |
Szepesi [39] |
13 |
6–24 |
6.1 |
113 |
0 |
ND |
98 grade I+II |
98 grade A+B |
Anterior approach + pelvic osteotomy |
Haidar [40] |
25.4 |
18–67 |
7.6 |
37 |
8.1 |
0 |
83.8 grade I+II |
97.3 MacKay grade A+B |
Anterior approach + Salter osteotomy |
Morcuende et al. [41] |
14 |
2–50 |
11 |
93 |
24 grade II; 14 grade III; 3 grade IV; 2 no classification Buchholz, Ogden |
2.2 |
71 grade I+II |
ND |
Anteromedial (Weinstein) |
Koizumi et al. [43] |
14 |
5–29 |
19.4 |
35 |
42.9 Kalamchi |
ND |
54.3 |
ND |
Ludloff, 50% reoperated |
Turner [44] |
11.2 |
2–25 |
8.1 |
56 |
8.9 |
ND |
98 grade I+II |
ND |
Medial approach 19% acetabular osteotomy |
Ryan et al. [45] |
76.8 |
36–108 |
10.6 |
25 |
44 grades I–III Salter, Buchholz, Ogden |
ND |
72 grade I+II |
ND |
Anterior approach Smith-Petersen + short osteotomy |
Akagi et al. [46] |
14 |
5–26 |
15 |
22 |
31.8 Kalamchi |
ND |
9.1 grade I; 54.5 garde II |
ND |
Smith-Petersen, no osteotomies until 15 years |
Olney et al. [47] |
29 |
15–117 |
3.6 |
18 |
5.5 |
0 |
100 grade I+II |
100 grade A+B |
Anterior approach VDO + pelvic osteotomy |
Cordier et al. |
14 |
3–48 |
15.3 |
118 |
6 Hirohashi et al. |
11 |
76 grade I+II CE 20–25?, 17% |
98 grade A+B |
Anterior approach (Tönnis), acetabular osteotomies |
Another possible complication that needs to be discussed is redislocation. In the literature (Tab. 8) redislocation occurred in 4% to 12%. For the sake of stabilisation of the femoral head a long girdle-like capsular flap was detached from the craniolateral redundant capsule, pulled anteriorly around the femoral head and sutured together with the previously incised capsule at the medial Joint border (Fig. 3).
If the acetabular angle had a pathological grade 3 and 4 of deviation from normal according to age (Tab. 1) acetabuloplasty with transiliac osteotomy was performed in combination with femoral head reduction in Order to lever the acetabular roof down laterally (Fig. 2 and 4). This way the labrum extends more laterally and distally over the femoral head and offers immediate stabilization.
There are different ways to improve the acetabular roof angle by osteotomies. Salter (28) and Pemberton (29) osteotomize in the anterior- to posterior direction, Wiberg, 1953, (10) in the lateral - to medial direction. In Salters osteotomy the distal pelvic fragment with the acetabulum in total is rotated antero-lateral around an axis passing through the pubic symphysis and the posterior part of the osteotomy. Therefore the improvement of the acetabular angle is limited and the acetabulum obtains a decreased anteversion (30). If this does not remodel, especially towards the end of growth, and the femoral anteversion is low in addition, pain and osteoarthrosis are to be expected (9).
The osteotomy from lateral in medial direction (Fig. 4), which we prefer, has the advantage that an Image intensifier can be used all the way and the chisel is directed exactly as wanted. The anterior part of the osteotomy is visible. Posteriorly we can feel the chisel slightly protruding in the sciatic notch and control it with the finger while it moves medially. The osteotomy ends medially shortly above the posterior end of the triradiate cartilage. In the bone and the anterior- to posterior part of the cartilage zone the acetabular roof can be bent down to the highest degrees (50°). Early fusions of the triradiate cartilage have not been observed (11-14).
In the first years acetabuloplasty was combined with varus-detorsion osteoftomy. We used the femoral bone wedge to support the acetabular roof. Later, when we avoided varus osteotomies as Salter does, xenogenic bone wedges of animals were introduced by Braun Co., Melsungen. Today bone wedges from allergenic femoral necks or femoral heads with a firm cortical rim are carefully examined and tested according to standardized bone bank rules and sterilized at 121°C for 20 min. and then kept deep frozen in the bone bank (31).
Conclusions
As our results show, open reduction of developmental dislocation of the hip can achieve in 92 % normal (CE angle >25°) or almost normal hips (20-25°) at the end of growth. The reduction through a ventral approach first lateral, then medial to the iliopsoas muscle, shortening osteotomy and other preventive measures to avoid ischemic necrosis are important. The advantages of the inguinal approach of Tönnis are:
- Optimal vision into the acetabulum before and after reduction from anteriorly. When dissecting the medial labrum and transverse ligament, trauma to the acetabular artery and vein is easier to avoid. Also, the deep reduction is better controlled than by lateral approaches.
- The operation is confined to the acetabulum and the inguinal region. The femoral neck is left covered. The iliopsoas tendon is obliqually dissected at the height of the pubis and acetabulum. Trauma to the medial femoral circumflex artery is avoided this way.
- Simultaneously a postero-lateral capsulorraphy and acetabular osteotomies can be performed from the same incision. Only subtrochanteric shortening osteotomies need a short lateral incision at the femur. This more distal shortenig does not impede the proximal femoral blond circulation. Detorsion-varus osteotomies have disadvantages (see chapter of technique of open reduction) and became very rare with our transiliac osteotomy technique close to Wiberg 1953.
- The abductor muscles have not been damaged as the minimal rate of limping shows in the evaluation.
- Medial approaches have a higher risk of ischemic necroses (16, 33-36) and need a second approach for acetabular osteotomies, which are frequently necessary in the second year of life and later, but sometimes even before. Postero-lateral capsulorraphies which are important for immediate stability cannot be performed from the medial approach.
- The iliac apophysis and pelvic wing should not be used as a bone wedge for acetabular osteotomies as Pemberton (29) has proposed it. This can result later in pelvic deformities and muscular functional deficiencies.
Simons (36) as well as Gabudza (37) stated that the indication for a certain operative approach should depend on the exact case. However, this does not apply to the approach described in this paper. Also, disadvantages of the ventral approach mentioned by Gabudza are not relevant for the approach laterally and medially to the iliopsoas muscle. Another advantage are the almost invisible scars in the inguinal region.
References
- Tönnis D. Der Leistenschnitt als Zugang zur operativen Hüftreposition. Z Orthop !978 116: 130-132.
- Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. With collaboration of H. Legal and R. Graf. New York: Springer, 1987.
- Tönnis D. Surgical treatment of congenital dislocation of the hip. Clin Orthop 1990; 258: 33-40.
- Tönnis D, Storch K, Ulbrich H. Results of newborn screening for CDH with and without sonography and correlation of risk factors. J Pediatr Orthop 1990; 10: 145-152.
- Tönnis D, Itoh K, Heinecke A, Behrens K. Die Einstellung der angeborenen Hüftluxation unter Arthrographiekontrolle, eine individuelle, risikoverringernde und zeitsparende Methode. Z Orthop 1984; 122: 50-61.
- Basset GS, Engsberg JR, McAlister WH, Gordon JE, Schoenecker PL. Fate of the psoasmuscle after open reduction for developmental dislocation of the hip.J Pediatr Orthop 1999; 19: 425-432.
- Damsin JP, Lazennec JY, Gonzales M, Guerin-Surville H, Hannoun L. Arterial supply of the acetabulum in the fetus: application to periacetabular surgery in childhood. Surg Radiol Anat 1992; 14: 215-221.
- Katthagen BD, Spies H, Bachmann G. Die arterielle Durchblutung der Hüftgelenkspfanne. Z Orthop 1995; 133: 7-13.
- Tönnis D, Heinecke A. Acetabular and femoral anteversion: Relationship with osteoarthritis of the hip. Current concepts review. J Bone Joint Surg 1999; 81-A: 1747-1770.
- Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg 1953; 35-A: 65-80.
- Brüning K, Heinecke A, Tönnis D. Technique and long-term results of acetabuloplasty. Acta Orthop Belgica 1990; 56: 287-292.
- Tönnis D, Brüning K, Heinecke A. Lateral acetabuloplasty. J Pediatr Orthop Part B 1994; 3: 40-46.
- Tönnis D. Treatment of residual dysplasia after developmental dysplasia of the hip as a prevention of early coxarthrosis. J Pediatr Orthop Part B 1993; 2: 133-144.
- Tönnis D. Lateral acetabuloplasty. In: M.F. Macnicol, editor. Color Atlas and Text of Osteotomy of the Hip. London: Mosby-Wolfe, 1995. pp. 31-38.
- Bonmann, R. Ergebnisse der Azetabuloplastik in der modifizierten Dortmunder Technik mit allogenen autoklavierten Knochenkeilen in einem postoperativen Zeitraum von 8 bzw. 9 Jahren. Inauguraldissertation, Univ. Giessen 2003.
- Tönnis D, editor. Congenital hip dislocation - Avascular necrosis. 1. Collective statistics prepared by the commission for the study of hip dysplasia of the GSOT. New York: Thieme-Stratton, 1982.
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand 1939; 83, Suppl. 83.
- Lequesne M, de Seze S. Le faux profil du bassin. Nouvelle incidence radiogra-phique pour l´etude de la hanche. Rev Rhum Mal Osteoartic 1961; 28: 643-652.
- Busse J, Gasteiger W, Tönnis D. Eine neue Methode zur röntgenologischen Beurteilung eines Hüftgelenkes - Der Hüftwert. Arch Orthop Trauma Surg 1972; 72: 1-9.
- Busse J, Gasteiger W; Tönnis D. Die Bedeutung des Hüftwertes für die Diagnose und Prognose deformierter Hüftgelenke. Arch Orthop Trauma Surg 1972; 72: 245-252.
- Tönnis D, Arning A, Bloch M, Heinecke A, Kalchschmidt K. Triple pelvic osteotomy. J Pediatr Orthop Part B 1994; 3: 54-67.
- Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed and arthrographic studies of recent cases. Acta Chir Scand 1941; 64: Suppl. 63.
- Gibson PH, Benson MKD. Congenital dislocation of the hip. Review at maturity of 147 hips treated by excision of the limbus and derotation osteotomy. J Bone Joint Surg 1982; 63-B: 169-175.
- Williamson DM, Glover SD, Benson MKD. Congenital dislocation of the hip pre-senting after the age of three years. J Bone Joint Surg 1989; 71-B: 745-51.
- Gamble JG, Mochizuki C, Bleck EE, Rinsky LA. Coxa magna following surgical treatment of congenital hip dislocation. J Pediatr Orthop 1985; 5: 528-33.
- Imatani J, Miyake Y, Nakatsuka Y, Akazawa H, Mitani S. Coxa magna after open reduction for developmental dislocation of the hip. J Pediatr Orthop Part A 1995; 15: 337-341.
- Hirohashi K, Kambara T, Narushima M, Lee Y, Shimazu A. A radiographic study of ischemic necrosis following the treatment of CDH. J Jpn Orthop Assoc 1982; 56: 927-928.
- Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg 1961; 43-Br: 518-539.
- Pemberton PA. Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg 1965; 47-A: 65-86.
- Dora C, Mascard E, Mladenov K, Seringe R. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop Part B 2002; 11: 34-39.
- Ekkernkamp M, Katthagen BD. Die Azetabuloplastik. Orthopäde 1997; 26: 75-80.
- Hefti F. Offene Repositionsverfahren. Orthopäde 1997; 26: 67-74.
- Kalamchi A, Schmidt TL, MacEwen GD. Congenital dislocation of the hip. Open reduction by the medial approach. Clin Orthop 1982; 169: 127-132.
- Koizumi W, Moriya H, Tsuchiya K, Takeuchi T, Kamegaya M, Akita T. Ludloffs medial approach for open reduction of congenital dislocation of the hip. A 20-year follow-up. J Bone Joint Surg 1996; 78-Br: 924-929.
- Morcuende JA, Meyer MD; Dolan LA, Weinstein SL. Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. J Bone Joint Surg 1997; 79-A: 810-817.
- Simons GW. A comparative evaluation of the current methods for open reduction of the congenitally displaced hip. Orthop Clin North America 1980; 11: 161-181.
- Gabuzda GM; Renshaw TS. Reduction of congenital dislocation of the hip. Current concepts review. J. Bone and Joint Surg 1992; 74-A: 624-631.
- Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg 1984; 66-A: 412-420.
- Powell EN, Gerratana FJ, Gage JR. Open reduction for congenital hip dislocation. The risk of avascular necrosis with three different approaches. J Pediatr Orthop 1986; 6: 127-132.
- Galpin RD, Roach JW, Wenger DR, Herring JA, Birch JG. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg 1989; 71-A: 734-741.
- Castillo R, Sherman FC. Medial adductor open reduction for congenital dislo-cation of the hip. J Pediatr Orthop 1990; 10: 335-340.
- Dhar S, Taylor JF, Jones WA, Owen, R. Early open reduction for congenital dis-location of the hip. J Bone and Joint Surg 1990; 72-B: 175-180.
- Mergen E, Adyaman S, Ömeroglu H, Erdemli B, Isiklar U. Medial open approach for congenital dislocation of the hip using the Ferguson procedure. Arch Orthop Trauma Surg 1991; 110: 169-172.
- Mankey MG, Arntz GT, Staheli LT. Open reduction through a medial approach for congenital dislocation of the hip. A critical review of the Ludloff approach in sixty- six hips. J Bone Joint Surg 1993; 75-A: 1334-1345.
- Sugimoto N, Terayama K, Fujioka F. Results of congenital dislocation of the hip joint with open reduction followed up to an age of fifteen years or more. Bull Hosp Jt Dis 1993-95; 53: 30-36.
- Doudoulakis J K, Cavadias A. Open reduction of CDH before one year of age. 69 hips followed for 13 (10-19) years. Acta Orthop Scand 1993 64: 188-192.
- Gulman B, Tuncay IC, Dabak N, Karaismailoglu N. Salters innominate osteotomy in the treatment of congenital hip dislocation: a long-term review. J Pediatr Orthop Part A, 1994; 14: 662-666.
- Michiels I, Schmitz B, Zimmermann K. Die offene Reposition nach Ludloff. Eine Nachuntersuchung unter besonderer Berücksichtigung der Hüftkopfnekrosen. Medizinisch-Orthopädische Technik 1994; 114: 87-96.
- Szepesi K, Biro B, Fazekas K, Szucs G. Preliminary results of early open reduc-tion by an anterior approach for congenital dislocation of the hip. J Pediatr Orthop Part B 1995; 4: 171-178.
- Haidar RK, Jones RS, Vergroesen DA, Evans GA. Simultaneous open reduc-tion and Salter innominate osteotomy for developmental dysplasia of the hip. J Bone Joint Surg 1996; 78-B: 471-476.
- Weinstein SL, Ponseti IV. Congenital dislocation of the hip - Open reduction through a medial approach. J Bone Joint Surg 1979; 61-A: 119-124.
- Tumer Y, Ward W T, Grudziak J. Medial open reduction for developmental dislocation of the hip. J Pediatr Orthop Part A 1997; 17: 176-180.
- Ryan M G, Johnson LO, Quanbeck DS, Minkowitz B. One-stage treatment of congenital dislocation of the hip in chidren three to ten years old. J Bone Joint Surg 1998; 80-A: 336-344.
- Akagi S, Tanabe T, Ogawa R. Acetabular development after open reduction for developmental dislocation of the hip. Acta Orthop Scand 1998; 69: 17-20.
- Olney B, Latz K, Asher M. Treatment of hip dysplasia in older children with a combined one-stage procedure. Clin Orthop 1998; 347: 215-223.
- Ludloff K. The open reduction of the congenital hip dislocation by an anterior in-cision. Am J Orthop Surg 1913; 10: 438-454.
Authors listed in Table 10
| Download | |
|---|---|
| Long-term results after open reduction of developmental hip dislocation by an anterior approach first lateral, then medial of the iliopsoas muscle | PDF (x.x MB) |
