Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Therapy in unilateral Sirenomelia: Report of one Case
© Prof. Dietrich Tönnis, M.D., Christoph Schildhauer, M.D., Manfred Schildhauer, M.D.
Alle im Text verwendeten Abbildungen lassen sich per Mausklick vergrößert darstellen! Am Ende des Textes finden Sie darüber hinaus ein PDF zum Download.
Summary
A 17 month old boy was referred to us with a unilateral sirenoid malformation in 1970. Besides urogenital and lumbosacral vertebral defects, the right knee was flexed 160° and the hip externally rotated and abducted. The thigh and calf were connected by a soft tissue bridge with the heel fixed to the ischial region. Arteriography showed that the foot and lower leg were supplied by the profunda femoris artery through the soft tissue bridge. The lower leg had only a very small supply from the popliteal artery. Therefore an amputation by disarticulation at the knee joint was performed. A few months later, in addition, the hip flexion contracture was released. The boy was taught to walk with a prosthesis. At the age of 31 years he has a sedentary job and is more troubled by his urogenital than his orthopaedic defects. He prefers to walk with crutches and since a few years no longer uses his prosthesis.
Introduction
The sirenoid malformation is a special form of caudal regression syndrome which follows damage to the human tail bud. In the pure sirens the caudal portions of the spine and spinal cord are missing. The urogenital system is variously malformed: often the external genitals are missing or rudimentary and are shifted dorsally. The distinctive feature is the total fusion of the legs (symmelia) also referred to as the mermaid syndrome. In some cases only the feet are attached to each other (sympodia) or one is missing (monopodia). The syndrome may affect one side only.
There are already about 330 reports about sirenomelia up until 1976 (1). Up to now, as far as we know, only descriptions of single cases and investigations on the etiology were given. Merely two papers presented recommendations for therapy (2, 3). In 1991 Guidera et al. published the first report of a successful operative separation of both legs in complete sirenomelia (3).
Probably in the most cases no possibilities were seen for improvement by orthopaedic surgery. A 31-year-long observation of a single patient with a surgically treated unilateral malformation therefore seems valuable.
Clinical course
In 1970 a 17 month old boy was referred to us because of a unilateral sirenoid malformation at the right side (Fig. 1 and 2). There was no relevant family history. The pregnancy had been normal.

(Fig. 1) 17 month old boy with unilateral sirenoid malformation of the right leg. The knee is extremely flexed. The upper and lower leg are connected by a soft tissue bridge. The heel is connected to the skin of the ischial region.
After birth an anus praeternatural (colostomy) had to be performed in our pediatric surgical department because of anal atresia (Dr. H. Würtenberger). There was also penile hypospadia penis. A testis was palpable on the left side only. During operation it was found that the right kydney and the right testis were absent.
On admission to our department we found that the right knee was flexed 160° while the hip was externally rotated and abducted. The upper and lower leg were connected by a firm soft-tissue bridge (Fig. 1 and 2). The skin of the heel was connected to the ischial region. Neurologically touch and pain sensation was absent below L 1. With galvanic stimulation only the adductor muscles responded.

(Fig. 4) The sacrum has a marked defect of the right side and the pelvis and the right leg show hypoplasia. The right hip is well centred.
The radiographic findings were: a butterfly and hemivertebra at L 4 and L5 (Fig. 3 and Fig. 4), a rightsided sacral defect with meningomyelocele, hypoplasia of the pelvic bones, the right femur and the tibia (Fig. 5 and Fig. 6).
The right foot had only four metatarsals (Fig. 6). The urogenital defects were also rightsided. There was no kidney and no testis and a penile hypospadius penis. Before treatment the question arose whether the leg was salvageable even though the muscles were paralysed and sensation absent.
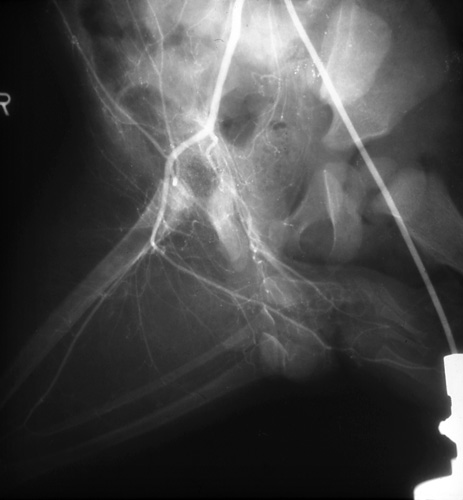
(Fig. 7) Arteriogram of the right common iliac artery, the internal and external iliac artery, the profunda and superficial femoral arteries. The internal liac artery continues to the heel, the profunda femoris to the dorsal side of the foot.
An arteriogram was performed via the left femoral artery. It was found that the right common iliac artery divided in the pelvis normally (Fig.7).
However, the internal iliac artery ran straight to the region of the symphysis and split into the soft tissue of the heel of the foot. The external iliac artery continued as the femoral artery. From this the profunda femoris artery arose and ran to the dorsal side of the foot.
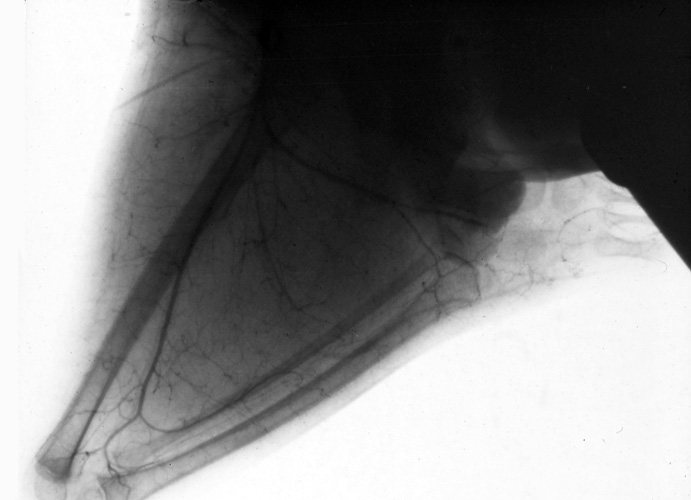
(Fig. 8) Division of the superficial femoral artery into a small branch to the fibula and into a popliteal artery with joint branches. In overprojection of the tibia there is apparently an anterior tibial artery. The posterior tibial and fibular artery are missing.
Another branch of the profunda femoris ran across the soft tissue bridge to the distal leg and into a branch accompanying the fibula (Fig. 8). The popliteal artery branched at the knee joint. Of the three normal large lower leg vessels expected, only the anterior tibial artery is seen over-lying the fibula.
Since the foot and parts of the lower leg were nourished only through vessels of the soft tissue bridge between the femur and the lower leg, they would be sacrificed by any straighting procedure of the leg. It was decided therefore to amputate the limb through the knee and use a prosthesis. Only the skeletal parts of the lower leg were removed through an incision at the anterior side of the tibia to maintain the soft tissue bridge and its vessels for the amputation stump. The lower leg and foot muscles had only a small number of muscle fibers. The postoperative course was uneventful.

(Fig. 9) After disarticulation of the knee the boy was supplied with a Thomas splint and a pelvic orthosis. The hip joint was fixed for walking because the muscles of hip and femur were paralysed.
Physical training for the contracture of the right hip joint and the muscles was started immediately. Nonetheless the muscles of the anterior and inferior iliac spine had to be released later to improve the flexion contracture. Due to the paralysis of the muscles of the hip and the femur a Thomas splint with a pelvic orthosis and an intermittent fixation of the hip joint was ordered (Fig. 9,10,11). This allowed the boy to stand up by himself after three months and to walk without any help after another two months.
At the age of 25 years he worked as a sedentary employee in industry. Although he wore his prosthesis to work, when at home he removed it and walked with crutches. His prosthetic usage decreased and by the age of 31 years he preferred to walk only with crutches. Proximal thigh muscles atrophy lead to repetitive soreness of the amputation stump. After a variety of urological operations he ended with a cutaneous urethrostomy which was complicated occasionally by infections. An ileum conduit is planned now. His colostomy is functioning well.
Discussion
The position of the right leg in a flexion-abduction contracture of the hip with the knee flexed and the foot connected to the anal region did not allow a normal sitting or walking for this boy. The thigh had to be brought in a normal position. The hip had to have at least a passive mobility allowing sitting and standing in a normal position, even if amputated. The remaining disadvantage was the paralysis of the hip and thigh muscles not allowing a normal gait and causing an atrophy of the muscles of the stump and an anaesthesia of the skin. Up to 25 years the patient used his prosthesis during daily work. But in the last years he felt very exhausted after his insufficient walking with the prosthesis due to the hip muscles paralysis. There is no active flexion, extension nor abduction.
Weightbearing by the atrophied stump also caused pain and soreness. Walking with crutches in comparison is not incommode for him. A higher amputation would not improve the situation. And a pelvic orthosis would interfere with the ileum conduit and the colostomy. His present prosthesis was only fixed to the shoulder. So it could not interfere with the colostomy and the cutaneous urethrostomy.
References
- Anton W, Stanulla H, Riefenstahl M. The problem of sirenoid malformation. Zentralbl Gynäkol 1976;98 (22):1394-400
- Carstens C, Marquardt E. Die operative Therapie schwerer Kniebeuge- und Hüftbeugekontrakturen beim kaudalen Regressionssyndrom.
Z Orthop 1988;126 (6) 625-8 - Guidera KJ, Raney E, Ogden JA, Highhouse M, Habal M. Caudal regression: A review of seven cases, including the mermaid syndrome.
J Pediatr Orthop 1991;11(6):743-7
| Download | |
|---|---|
| Therapy in unilateral Sirenomelia: Report of one Case |
PDF (1.3MB) |





