Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Triple Pelvic Osteotomy
© Prof. Dr. med. Dietrich Tönnis
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
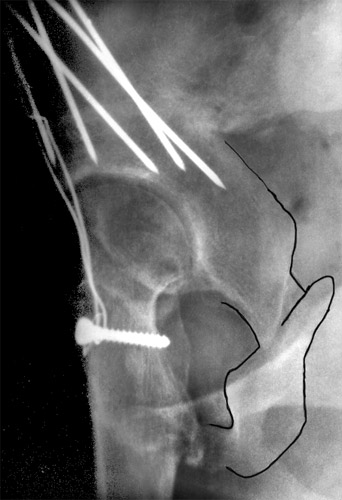
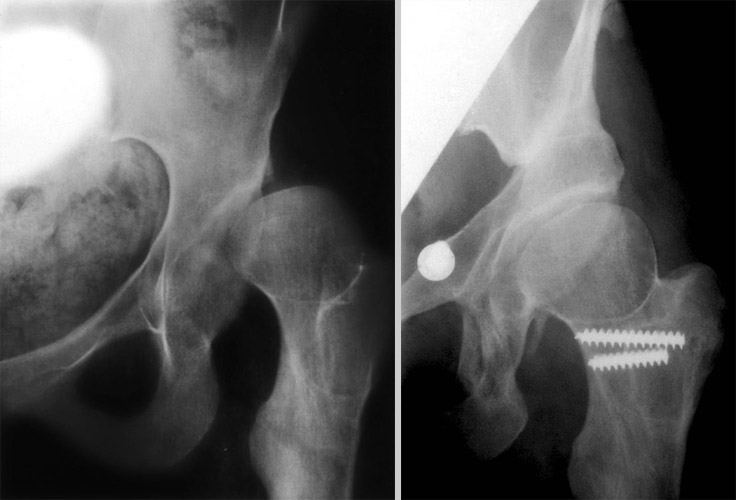
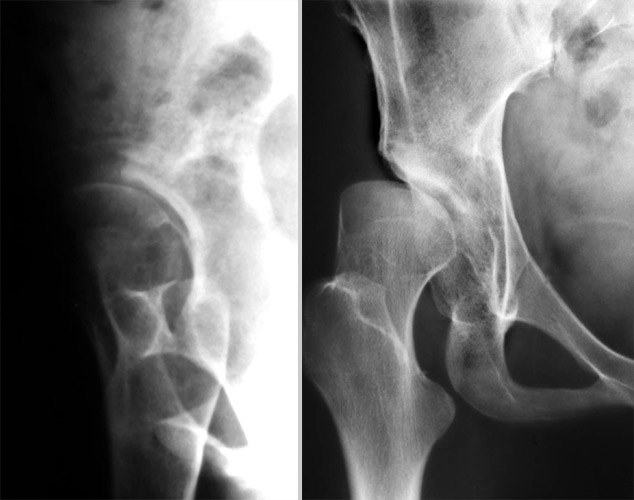
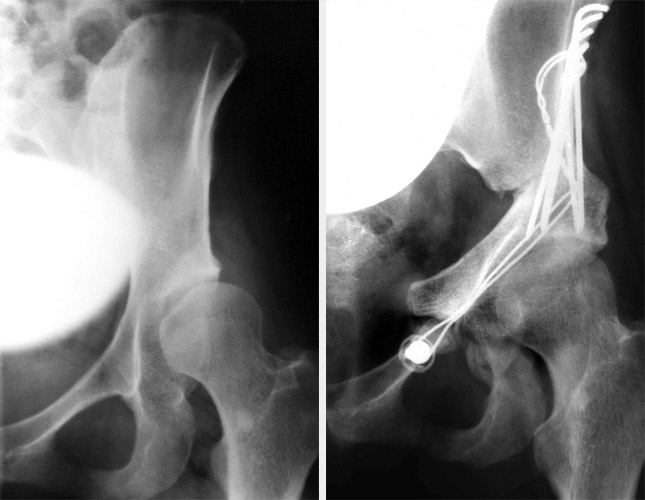
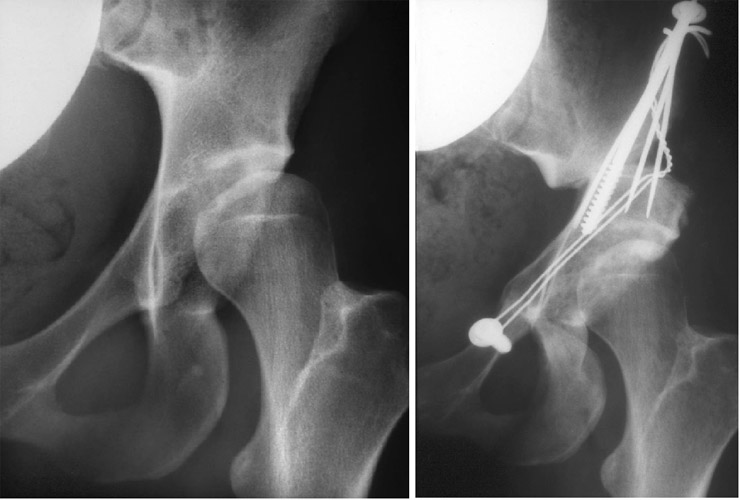
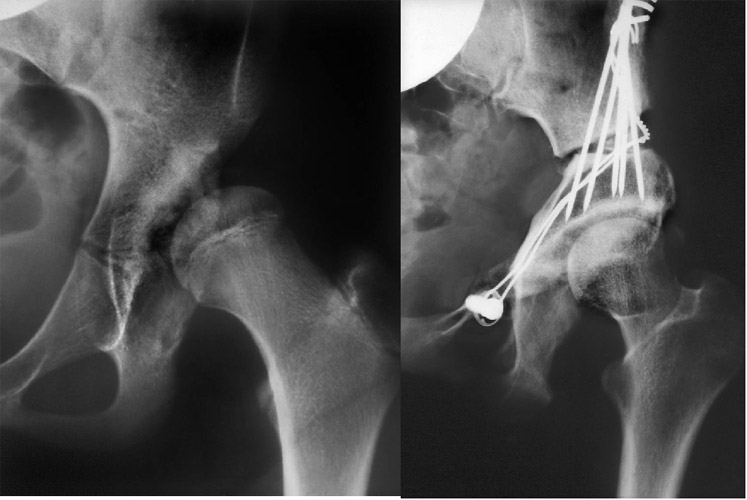
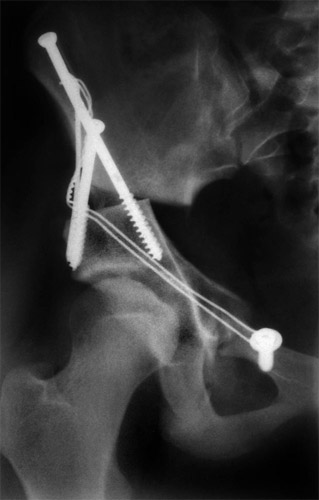
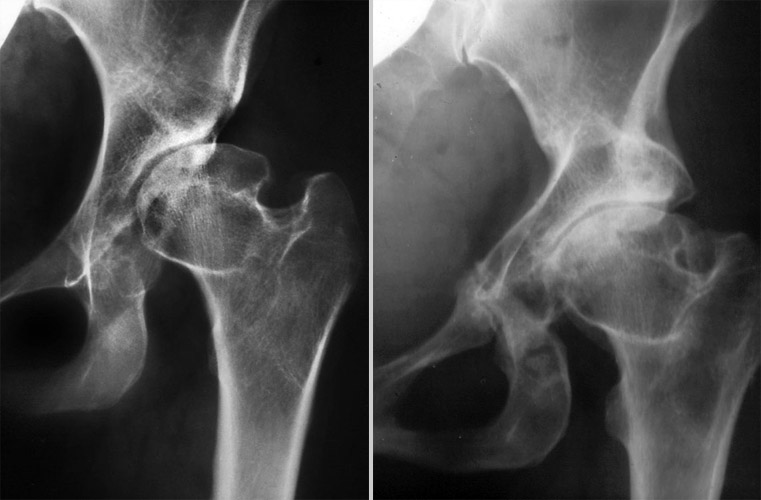
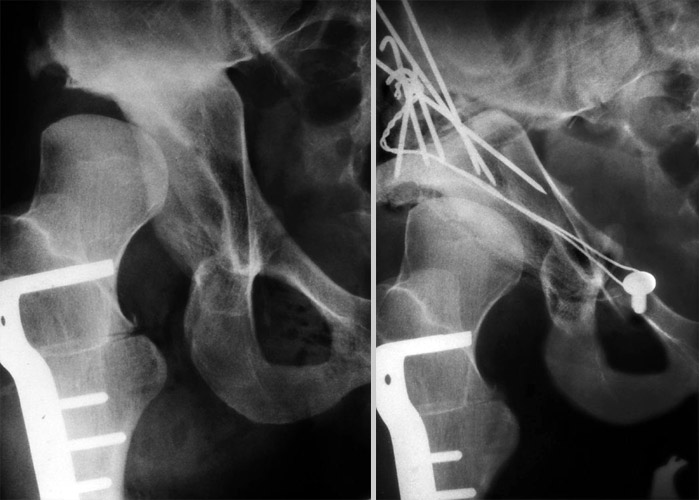
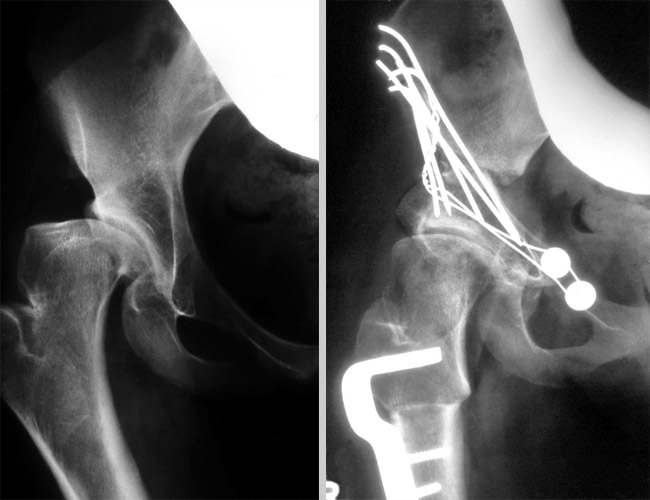
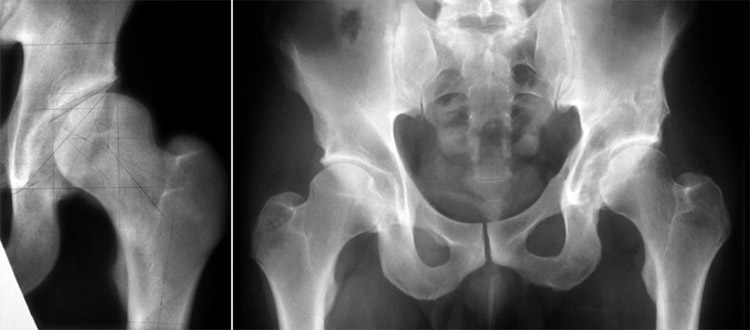
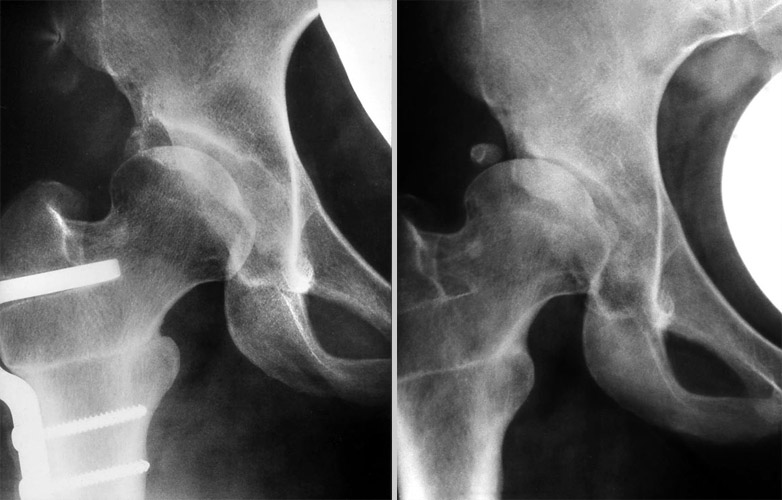 For a long time, developmental hip dysplasia in adolescents and adults, has been treated only by varus osteotomies according to the principles of Pauwels and Maquet. In this 25 year old woman you see the joint at the left, shortly after operation, and at the right 11 years later.
For a long time, developmental hip dysplasia in adolescents and adults, has been treated only by varus osteotomies according to the principles of Pauwels and Maquet. In this 25 year old woman you see the joint at the left, shortly after operation, and at the right 11 years later.
The joint space laterally is worn off. The weightbearing area was too small and did not cover the femoral head neither broad enough nor horizontal. Therefore the pressure of the load was too high.
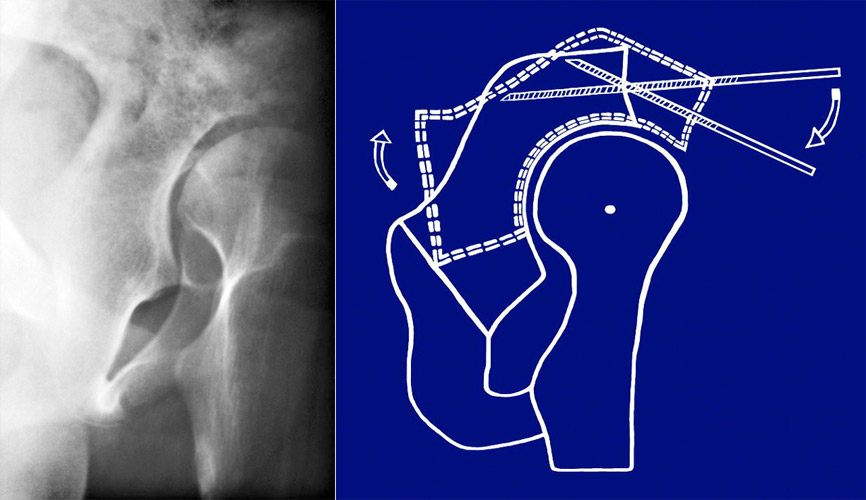
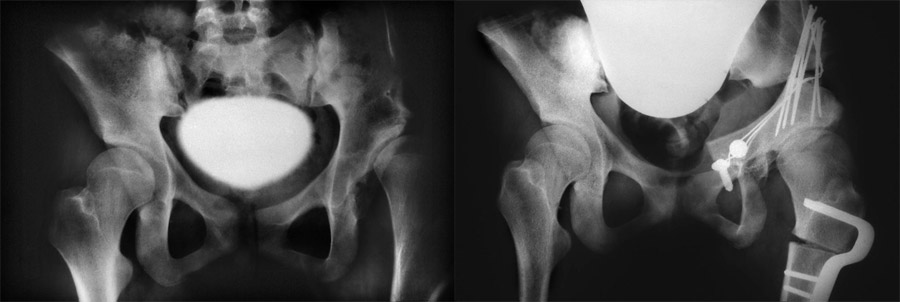
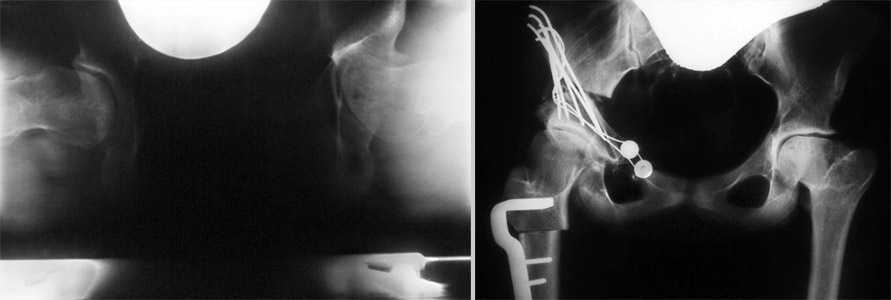
 This can only be corrected by a rotation of the whole acetabulum as you see here after the triple pelvic osteotomy as we perform it.
This can only be corrected by a rotation of the whole acetabulum as you see here after the triple pelvic osteotomy as we perform it.
In the last 40 years different techniques of acetabular rotation have been described. This is the antero-posterior view.
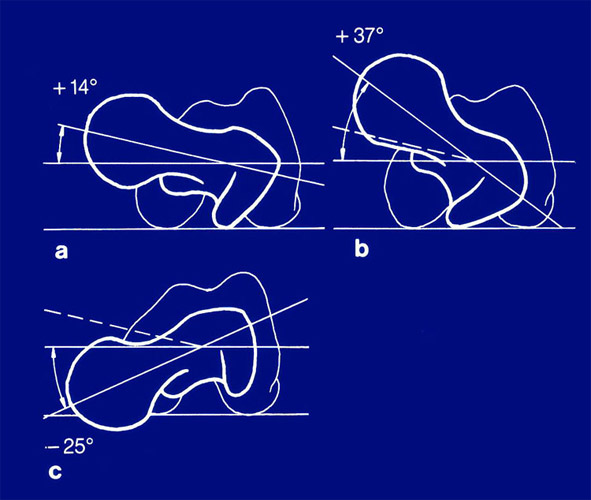
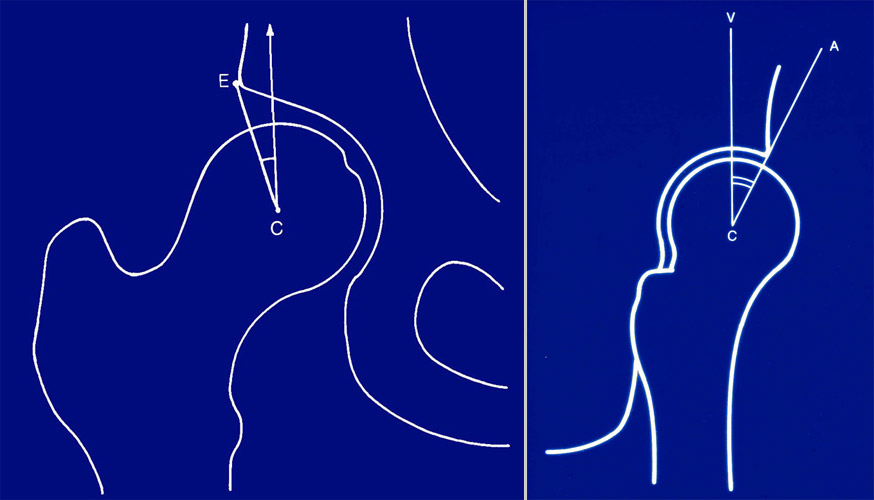
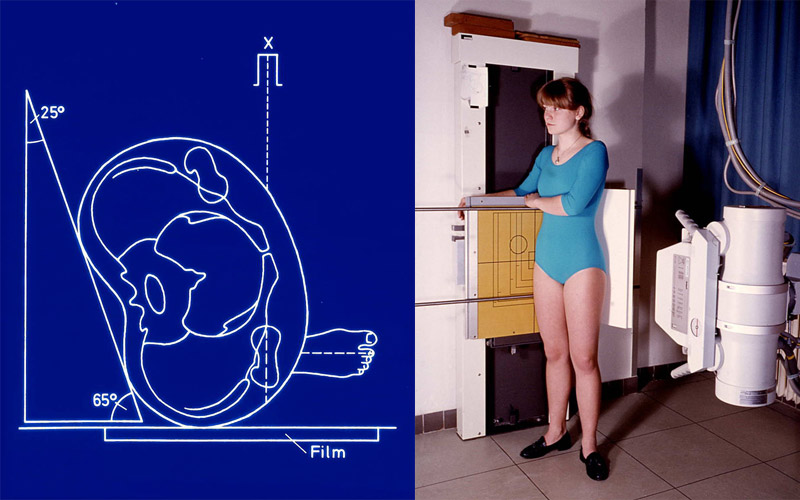 The lateral view of the joint, the second plane, we do obtain with the so called "false profile radiography" of Lequesne and de Seze.
The lateral view of the joint, the second plane, we do obtain with the so called "false profile radiography" of Lequesne and de Seze.
In this case the patient turns back 25° so that we get a lateral picture of the anterior coverage of the hip, which stands here more anteriorly.
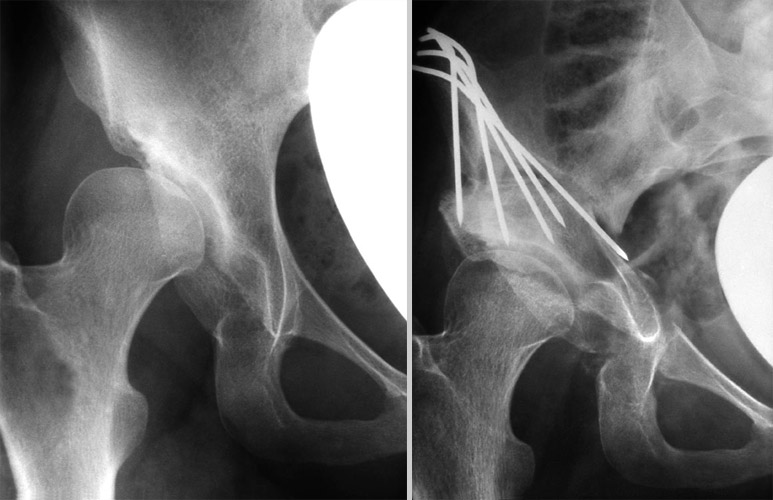
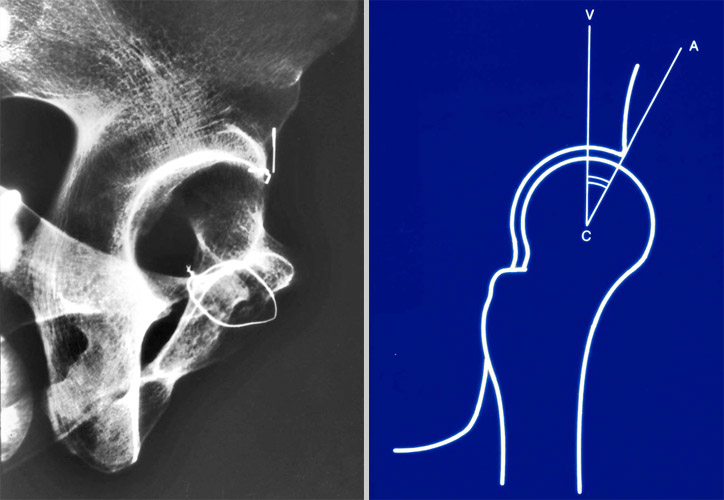 At the left I present a radiography of a normal skeleton. The anterior margin of the acetabulum is marked with a horizontal wire. At the right the VCA or "anterior CE angle" is demonstrated.
At the left I present a radiography of a normal skeleton. The anterior margin of the acetabulum is marked with a horizontal wire. At the right the VCA or "anterior CE angle" is demonstrated.
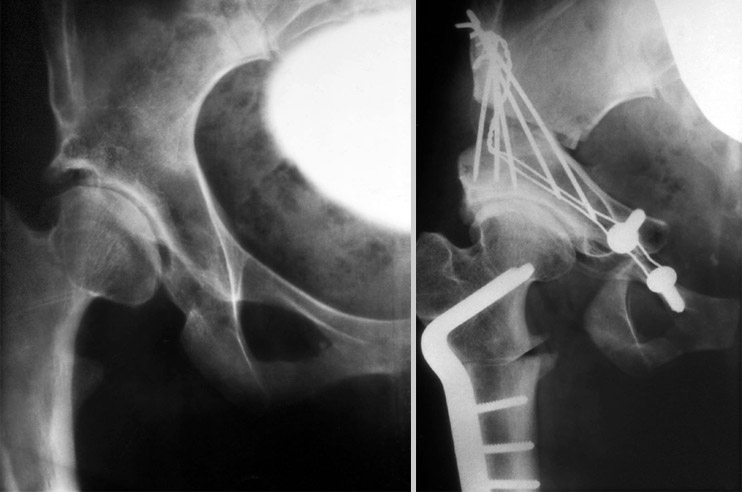
 This picture shows a severe dysplasia. We find the acetabular rim anteriorly at the end of the bright sclerotic line. Up to here we measure the anterior CE angle. It is severely decreased down to a few negative degrees. The normal angle is 25 to 30 degrees. But the femoral head has not yet shifted upwards and anteriorly. The lower margin of the femoral head is found here at the same hight as the lower acetabular margin.
This picture shows a severe dysplasia. We find the acetabular rim anteriorly at the end of the bright sclerotic line. Up to here we measure the anterior CE angle. It is severely decreased down to a few negative degrees. The normal angle is 25 to 30 degrees. But the femoral head has not yet shifted upwards and anteriorly. The lower margin of the femoral head is found here at the same hight as the lower acetabular margin.
In this case a higher dislocation of the femoral head is apparent considering the distance between the lower margin of the femoral head and the lower margin of the acetabulum. At the right the dislocation in the ap-view is shown for comparism.
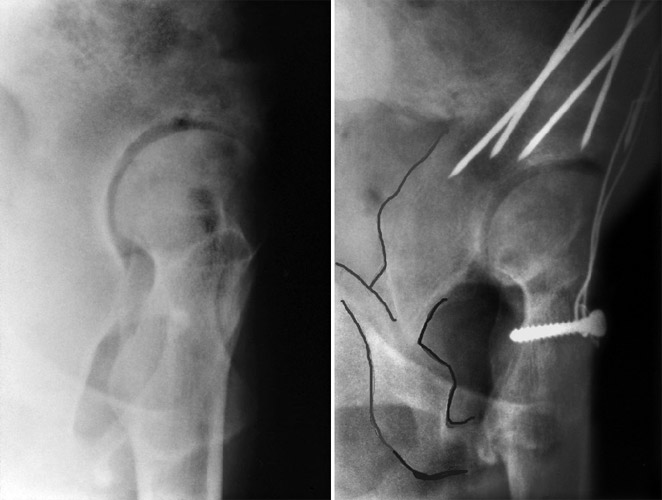
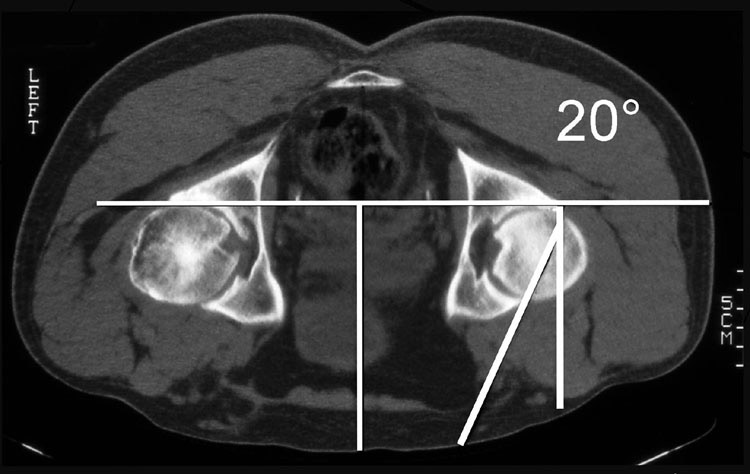
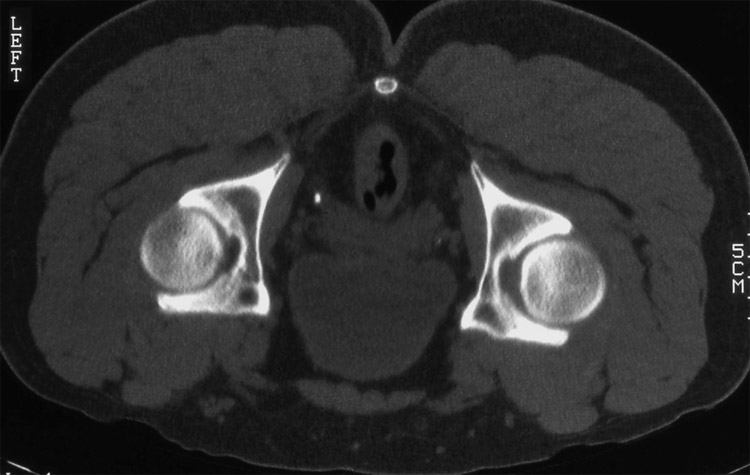
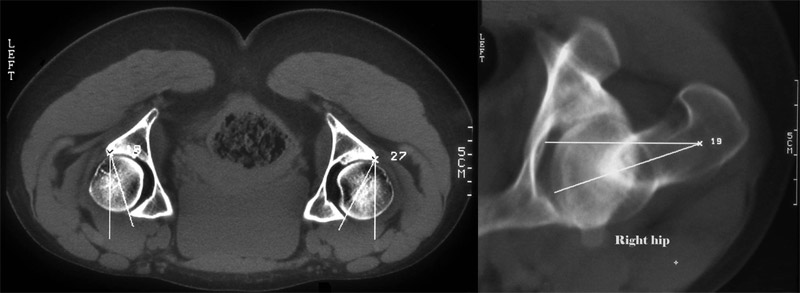 The third plane is the horizontal, in which we measure the acetabular and femoral anteversion. It is normally 15 to 20° for both angles.
The third plane is the horizontal, in which we measure the acetabular and femoral anteversion. It is normally 15 to 20° for both angles.
This plane we evaluated in later years, because we found problems there additionally.
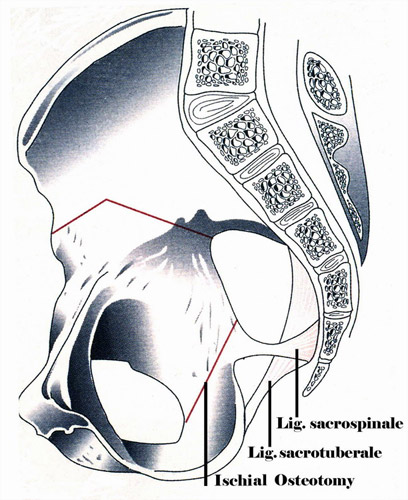
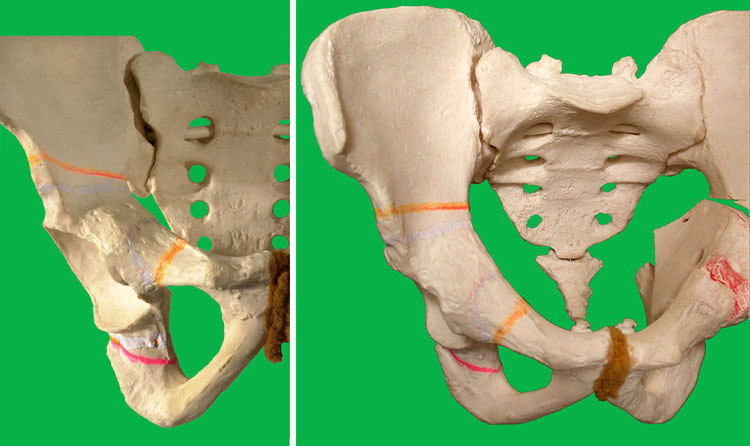
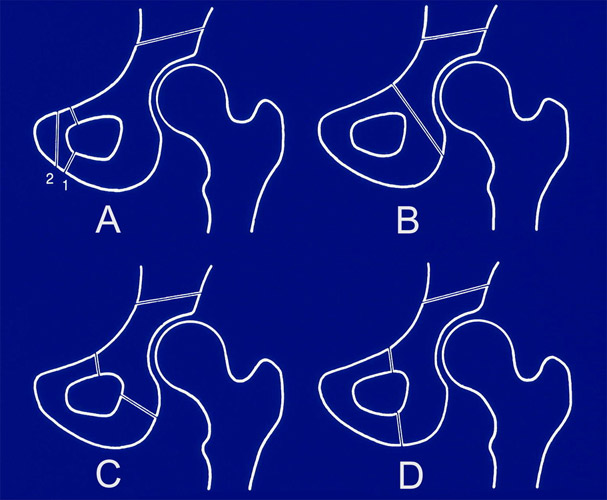 Many different osteotomies have been described since LeCoer 1965 and Hopf (1966) began with the first ones. They differ regarding the distance of the acetabulum and whether they release the acetabulum from the sacroischial ligaments or not. When the distance is too large like in Fig. A, the rotation is very limited.
Many different osteotomies have been described since LeCoer 1965 and Hopf (1966) began with the first ones. They differ regarding the distance of the acetabulum and whether they release the acetabulum from the sacroischial ligaments or not. When the distance is too large like in Fig. A, the rotation is very limited.
When ilium and ischium are osteotomized together as in Fig. B, the teardropfigure and the onlying acetabular vessels will be cut. Osteonecrosis can follow.
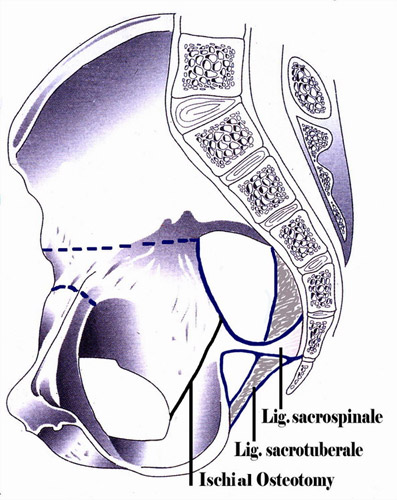
In Fig. C the sacrospinal ligament and in Fig. D. additionally the sacrotuberal ligament are limiting the acetabular rotation. Our osteotomy could be placed under letter C, but it is an oblique, not a transverse osteotomy of the ischium.
Prof. Ganz later came to the same result by a "periacetabular osteotomy" also in front of the two ligament insertions.
 We started with our technique in 1976. During the course of time the technique has been further elaborated in different ways. First we placed the patient into a prone position for the ischial osteotomy, which is easier for the beginning.
We started with our technique in 1976. During the course of time the technique has been further elaborated in different ways. First we placed the patient into a prone position for the ischial osteotomy, which is easier for the beginning.
Now we place him in a lateral position and can turn him then without further draping into a slightly prone position for the ischial osteotomy and a supine position for the pubic and the ilium osteotomy. The table is radiolucent.
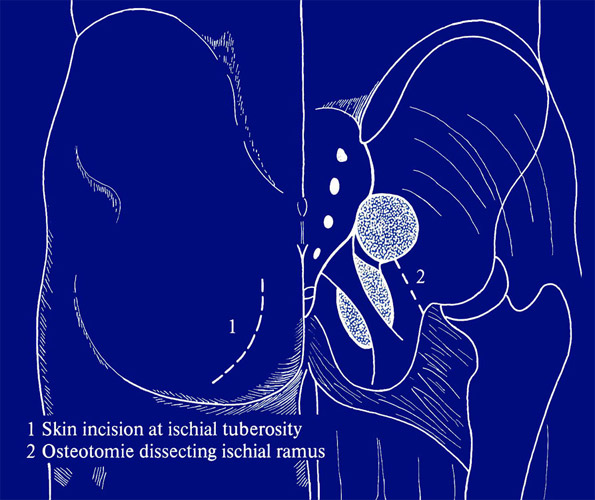 For the ischial osteotomy we palpate the ischial tuberosity and from there the sacrotuberal ligament. The incision is made parallel to the ligament. The fibers of the glutaeus maximus muscle are bluntly separated longitudinally.
For the ischial osteotomy we palpate the ischial tuberosity and from there the sacrotuberal ligament. The incision is made parallel to the ligament. The fibers of the glutaeus maximus muscle are bluntly separated longitudinally.
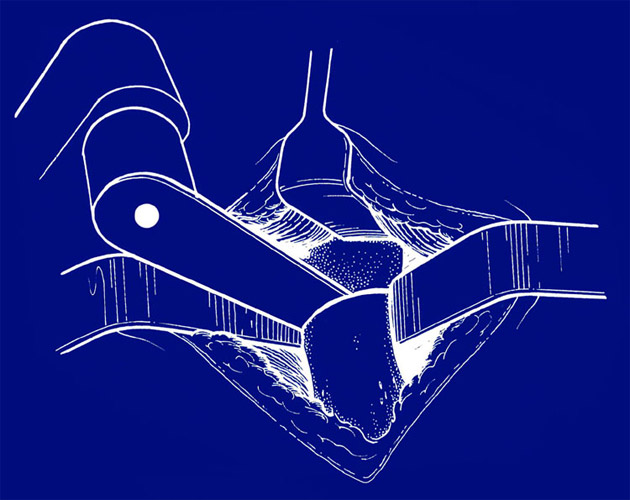
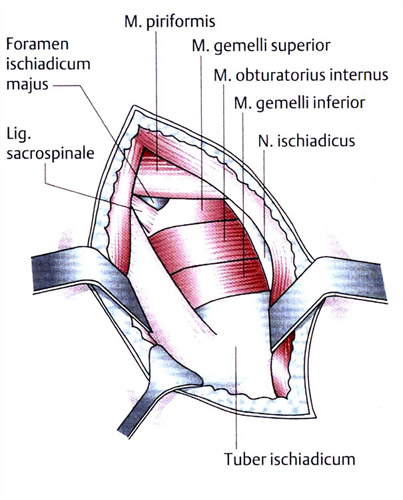 The ischial tuberosity is prepared first. Proximally, the small external rotator muscles are covering the ischium. The sciatic nerve is shown medially in the drawing, but we leave him covered by muscles during the operation. Every stronger pressure of retractors should be avoided.
The ischial tuberosity is prepared first. Proximally, the small external rotator muscles are covering the ischium. The sciatic nerve is shown medially in the drawing, but we leave him covered by muscles during the operation. Every stronger pressure of retractors should be avoided.
The tendons of the small external rotators underneath are cut.
 Then a small retractor is pushed beneath the muscles and placed into the sciatic notch lateral from the ischial spine, holding back these muscles. Now we are able to see the whole posterior part of the ischium.
Then a small retractor is pushed beneath the muscles and placed into the sciatic notch lateral from the ischial spine, holding back these muscles. Now we are able to see the whole posterior part of the ischium.
The ischial osteotomy should be long and oblique to guarantee consolidation after the anterior rotation of the acetabulum. With a smaller chisel we start the osteotomy at the sciatic notch. Here the bone is relatively thin and the blade of the chisel can be palpated underneath and redirected before it approaches or enters the joint.
 Two retractors are placed in the obturator foramen and a second broader chisel should be directed towards them. As a rule, we say that the chisel should be directed 20 to 30° anteriorly as seen at the right and towards the central longitudinal axis.
Two retractors are placed in the obturator foramen and a second broader chisel should be directed towards them. As a rule, we say that the chisel should be directed 20 to 30° anteriorly as seen at the right and towards the central longitudinal axis.
A chisel with less than 20° of anterior direction will run parallel to the obturator foramen. Rotation is not possible then. And with a direction of much more than 30° the chisel gets into the acetabulum.
Afterwards we have to control whether the osteotomy is complete. The sharp inner bony rim of the obturator foramen is sometimes not osteotomized between the two retractors.
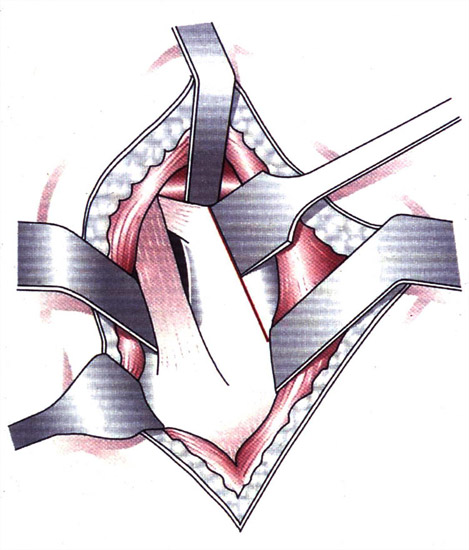
 The easiest way to approach the pubis is from the medial side of the joint, where it can be palpated. One must only take care not to proceed too far laterally, thus damaging the femoral vein. The pectineus muscle is released from the pubis. Retractors have to protect the obturator artery. For the osteotomy we use a small oscillating saw with water cooling.
The easiest way to approach the pubis is from the medial side of the joint, where it can be palpated. One must only take care not to proceed too far laterally, thus damaging the femoral vein. The pectineus muscle is released from the pubis. Retractors have to protect the obturator artery. For the osteotomy we use a small oscillating saw with water cooling.
 Frequently we think it is neccessary to perform a medial displacement of the joint for biomechanical reasons. Then the pubic osteotomy is inclined medially and dorsally.
Frequently we think it is neccessary to perform a medial displacement of the joint for biomechanical reasons. Then the pubic osteotomy is inclined medially and dorsally.
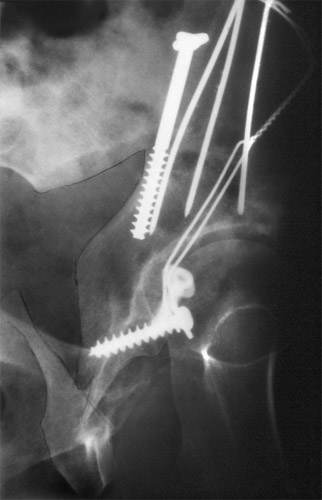
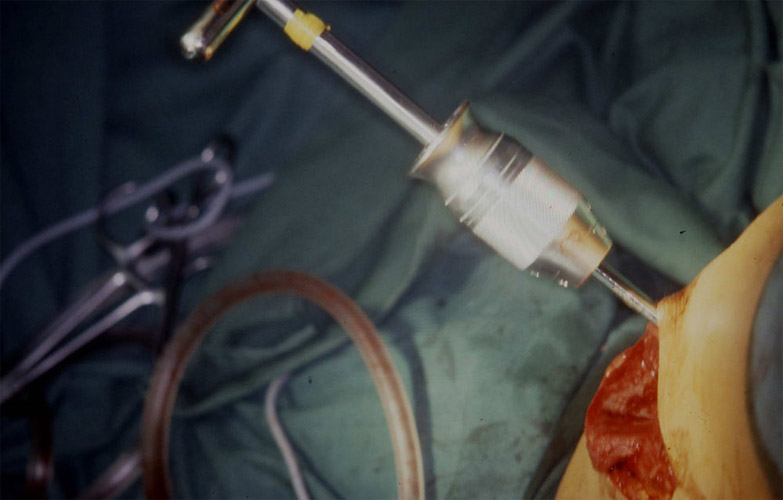 The plane of the ilium osteotomy is established under image intensifier control, when we insert a 5 mm Schanz screw with a handle for acetabular rotation.
The plane of the ilium osteotomy is established under image intensifier control, when we insert a 5 mm Schanz screw with a handle for acetabular rotation.
 It is inserted 45° from anterolateral and not less than a centimeter above the acetabular roof. Today the osteotomy is performed 2 centimeters above the Schanz screw to give hold for 2 screws coming from the iliac crest.
It is inserted 45° from anterolateral and not less than a centimeter above the acetabular roof. Today the osteotomy is performed 2 centimeters above the Schanz screw to give hold for 2 screws coming from the iliac crest.
 We have first performed the ilium osteotomy from lateral. Later Dr. Kalchschmidt, my former colleague, performed it from the inner side of the pelvis to avoid trauma to the medial gluteus muscle and the vessels of the pelvis laterally.
We have first performed the ilium osteotomy from lateral. Later Dr. Kalchschmidt, my former colleague, performed it from the inner side of the pelvis to avoid trauma to the medial gluteus muscle and the vessels of the pelvis laterally.
Furtheron he performs the osteotomy now anteriorly inclined with an angle of 40° as seen here. The advantage is, that there is no bigger gap after anterior rotation, which would require more bone chips.
First we mark the ilium osteotomy with a chisel. Then we use a Tuke oscillating saw and water cooling. In the sciatic notch a longer retractor is protecting the sciatic nerve.
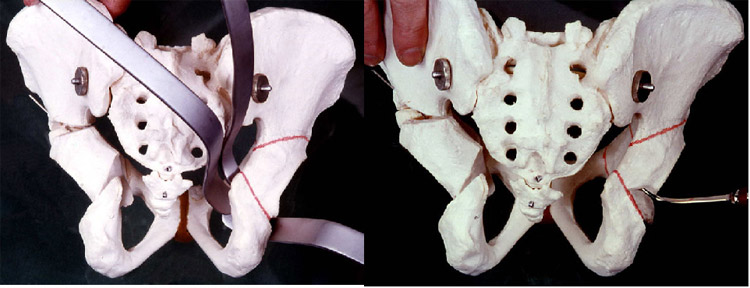
 A few words are necessary on the rotation of the acetabulum in 3 planes. Here you see what I mean as far as free rotation of the acetabulum with the Steinmann pin is concerned.
A few words are necessary on the rotation of the acetabulum in 3 planes. Here you see what I mean as far as free rotation of the acetabulum with the Steinmann pin is concerned.
The lateral part of the os pubis should be rotated upwards above the medial part of the pubis and then be medialized to place the joint more towards the center of gravity thus diminishing its load.

The lateral rotation we compare by looking at the position of the teardrop figure and the weight bearing area. In these false acetabulae we have to rotate the longest way.
There are of course other joints like this one, where only a slight hinging or rotation is sufficient and overcorrection should be avoided. With the years we introduced more and more the lateral rotation combined with medialization to diminish the load.
 In the second plane we have already seen that there are frequently great deficits in the anterior coverage of the femoral head. In this case, as well, the job is not done by only pulling the anterior part of the acetabulum distally.
In the second plane we have already seen that there are frequently great deficits in the anterior coverage of the femoral head. In this case, as well, the job is not done by only pulling the anterior part of the acetabulum distally.
As the drawing at the right side shows we have to turn the posterior part of the acetabulum upwards with the Schanz screw and rotate it in total. Its lower part has to glide upwards on the plane of the osteotomy. This is demonstrated here at the right side.
 This is a picture of how it should not be done. Only the upper part of the acetabulum is inclined or levered down anteriorly and the lower margin has not moved upwards and posteriorly on the osteotomy plane.
This is a picture of how it should not be done. Only the upper part of the acetabulum is inclined or levered down anteriorly and the lower margin has not moved upwards and posteriorly on the osteotomy plane.
Now there is a bigger gap in the ilium osteotomy and pseudarthroses may develop.
 The problems of the third plane we have not realized in the beginning of the triple osteotomy. My third paper will deal specially with decreased acetabular and femoral anteversion, because they can also cause pain, impingement and osteoarthrosis.
The problems of the third plane we have not realized in the beginning of the triple osteotomy. My third paper will deal specially with decreased acetabular and femoral anteversion, because they can also cause pain, impingement and osteoarthrosis.
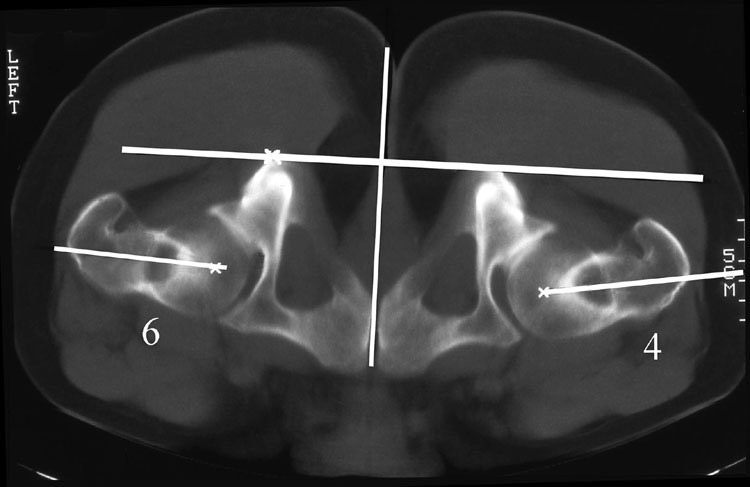 At the same time the femoral anteversion is decreased. Femoral anteversion is measured between a tangent dorsally at the femoral condyles of the knee and a line through the midst of the femoral neck and the center of the femoral head as seen here. In this horizontal plane we have to rotate the acetabulum and the femoral neck to a normal anteversion of 15 to 20°.
At the same time the femoral anteversion is decreased. Femoral anteversion is measured between a tangent dorsally at the femoral condyles of the knee and a line through the midst of the femoral neck and the center of the femoral head as seen here. In this horizontal plane we have to rotate the acetabulum and the femoral neck to a normal anteversion of 15 to 20°.
 But there is still another problem in this plane. We noticed for a long time, that the internal rotation of the hip was decreased to some degree after triple osteotomy. So we tried to rotate the acetabulum a bit internally when we fixed it. Then we found the papers of Anda and of Visser.
But there is still another problem in this plane. We noticed for a long time, that the internal rotation of the hip was decreased to some degree after triple osteotomy. So we tried to rotate the acetabulum a bit internally when we fixed it. Then we found the papers of Anda and of Visser.
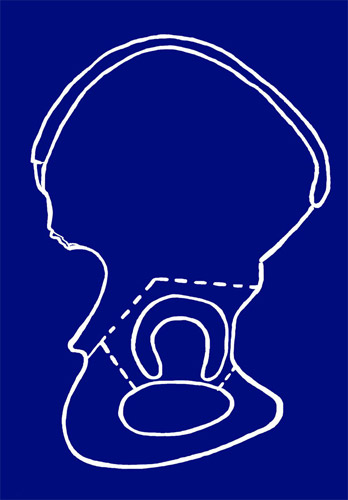
They showed experimentally that acetabular anteversion decreases with anterior pelvic inclination and increases with less inclination. At the left, you are able to look into the acetabulum. At the right, the pelvis is inclined anteriorly and the anterior margin now is reaching more laterally. This way acetabular anteversion is decreased to zero.

Here, at the left, we see a joint in which the upper anterior margin of the acetabulum also overlaps the posterior. Anteversion is partially decreased. After operation this overlaps even more. Some colleagues think that there is a good ventral coverage, but this is a misjudgement.
As far as this patient is concerned, postoperatively, the anterior margin overlaps the posterior to a great extent.
But the lateral radiography shows in two pictures that there was only a limited anterior coverage. Therefore the overlaping anterior margin is only a sign of decreased anteversion.
 Before acetabular rotation starts we recommend to put a short vertical K-wire in the acetabular roof to maintain control.
Before acetabular rotation starts we recommend to put a short vertical K-wire in the acetabular roof to maintain control.
After lateral and anterior rotation one should always rotate the acetabulum 15-20° internally and after a primary fixation examine the internal rotation of the hip in a position of 45° of flexion.
It should not be decreased. Anterior flexion of the acetabulum decreases the anteversion.
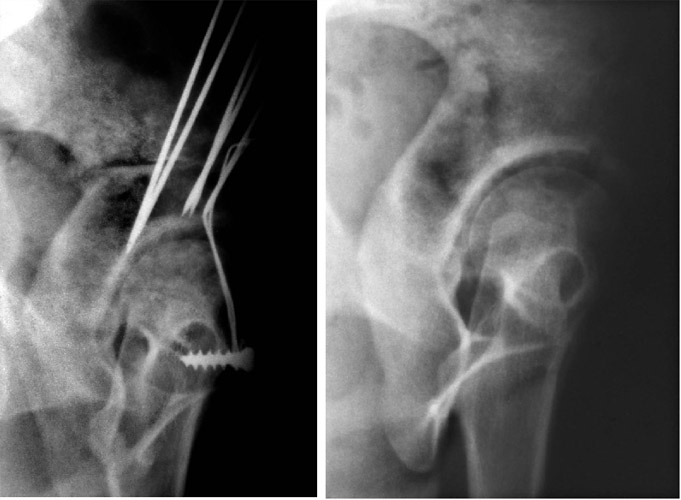
 In the beginning we performed the fixation of the ilium-osteotomy with K-wires, later with 2 or 3 screws. For the osteotomy of the pubis we used a cerclage around a screw at the medial pubis and a K-wire or screw laterally.
In the beginning we performed the fixation of the ilium-osteotomy with K-wires, later with 2 or 3 screws. For the osteotomy of the pubis we used a cerclage around a screw at the medial pubis and a K-wire or screw laterally.
The wire is put subperiostally on the pubis and pelvis underneath the muscles.
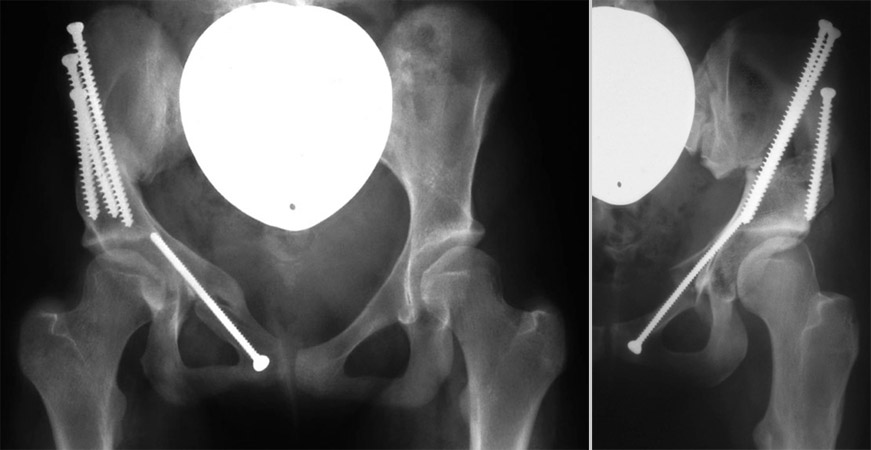
At present Kalchschmidt uses screws also for the pubis-osteotomy. The rotation and fixation of the acetabulum is performed under image intensifier control.
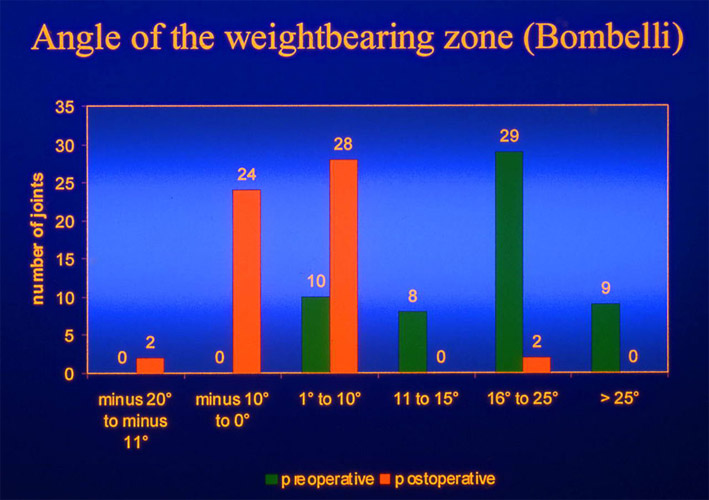
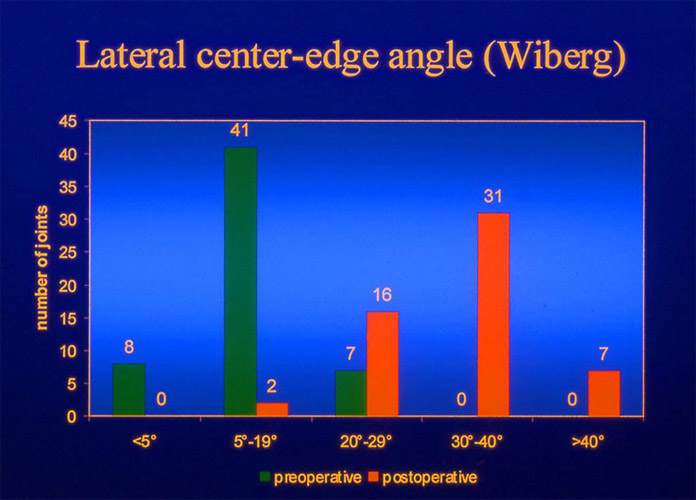
The question arises: which is the best position? Our answer is: the best angle causes no pain or only minimum pain. We evaluated this fact at a reexamination. We measured the following angles here: the CE angle of Wiberg and the VCA angle of Lequesne and de Seze, shortly called anterior CE angle.
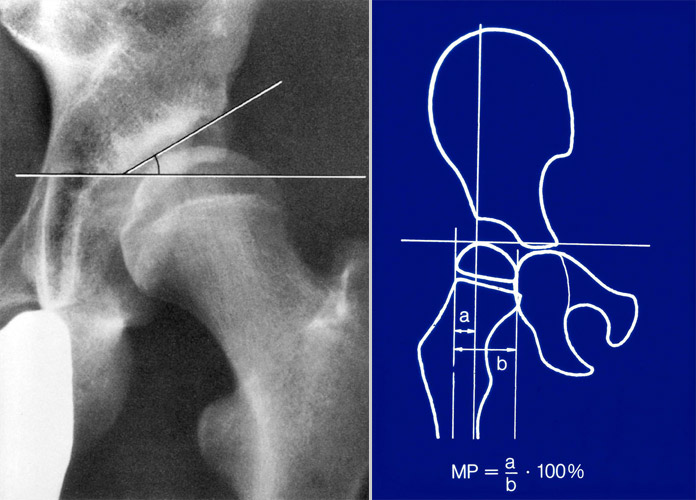
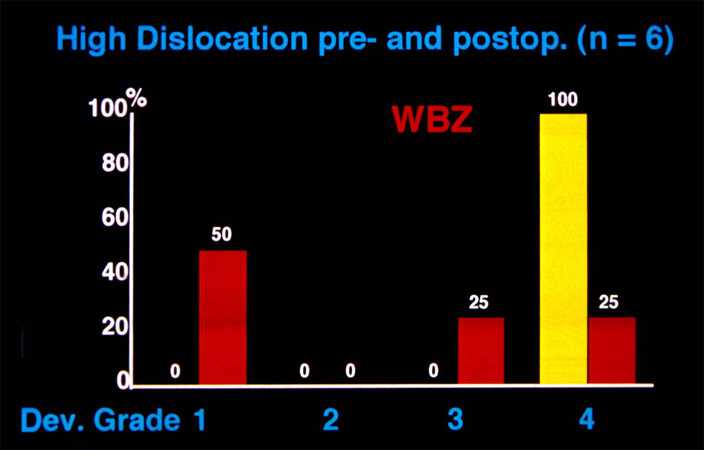
Furthermore the angle of the weightbearing zone of Bombelli at the left and the migration percentage of Reimers at the right.
| CE angle | No pain (%) | Total (n) |
|---|---|---|
| < 10 | 57.7 | 26 |
| 10 – 20 | 40.0 | 30 |
| 20 – 25 | 62.5 | 24 |
| 25 – 30 | 50.0 | 20 |
| 30 – 35 | 78.1 | 32 |
| 35 – 40 | 65.5 | 29 |
| > 40 | 63.6 | 11 |
| CE angle | no pain (%) | Total (n) |
|---|---|---|
| < 10 | 39.3 | 33 |
| 10 – 20 | 50.0 | 30 |
| 20 – 25 | 56.0 | 25 |
| 25 – 30 | 70.0 | 30 |
| 30 – 35 | 77.3 | 22 |
| 35 – 40 | 80.0 | 10 |
| > 40 | 68.2 | 22 |
The percentage of no pain in the CE and VCA angle is seen in the middle column. The highest percentage of both angles for no pain was found at 30° to 35°.
| WBZ angle | No pain (%) | Total (n) |
|---|---|---|
| < -5 | 50.0 | 6 |
| -5 - +5 | 74.1 | 58 |
| 6 – 10 | 66.7 | 33 |
| 11 – 15 | 45.0 | 20 |
| 16 - 25 | 44.7 | 38 |
| 26 – 55 | 52.9 | 17 |
| Migration % | No pain (%) | Total (n) |
|---|---|---|
| < 10 | 55.6 | 27 |
| 10 – 15 | 87.9 | 33 |
| 15 – 20 | 55.3 | 38 |
| 20 – 25 | 58.6 | 29 |
| 25 – 35 | 42.3 | 26 |
| > 35 | 56.3 | 16 |
The most important angle is the one of the weight bearing zone, because it is the best indicator for the actual size of the load bearing area. The optimal angle lies between minus and plus 5°, so practically at zero. This is our aim in the ap radiography. The migration percent has its optimum at 10-15% protruding under the acetabular roof. In this contact it is interesting, that zero is not the best value. This is the same, regarding the other values: at overcorrection the percentage of no pain decreases, which means pain is increasing.
VCA angle |
30 – 35° |
|---|---|
CE angle |
30 – 35° |
Loading zone angle |
-5 – 5° |
Migration (%) |
66.7 |
CE angle |
> 40° |
|---|---|
VCA angle |
> 40° |
Loading zone angle |
< -10° |
Migration % |
< 10 |
So we found optimal values and values of overcorrection.
| 1 | 2 | 3 | 4 | |
| Degrees | normal | mildly pathological | severely pathological | extremely pathological |
| CE angle | ≥ 30 | 20 – 29 | 5 – 19 | < 5 |
| VCA angle | ≥ 25 | 20 – 24 | 5 – 19 | < 5 |
| ACWZ angle | ≤ 9 | 10 – 15 | 16 - 25 | > 25 |
| Reimers Ind. | ≤ 15 | 16 – 25 | 26 – 40 | > 40 |
| Hip Value | < 16 | 16 – < 21 | 21 – < 31 | ≥ 31 |
For the evaluation of results we defined normal values and grades of deviation : mildly, severely and extremely pathological. Actually overcorrection should be added.
| Material |
|---|
| 351 patients operated 1977- 1987 |
| 197 patients reinvestigated |
| 216 joints operated, 19 bilaterally |
| 1 death by embolism |
Reinvestigations were performed at different times. One contained the unselected early material operated between 1977 and 1987 and reinvestigated between 5 and 16 years.
216 joints of 197 patients could be reinvestigated. 78 operations had been peformed on children and adolescents and 138 on adults.

The deformations of the joints were quite different. Therefore we introduced four grades of decentration. In grade 1 here the joint is fairly centered and spherical and best results can be expected.

In grade 2 the femoral head is dislocated in an elongated acetabulum, but can be recentered with a good rotation.

This is another grade 2 decentration. It is amazing that 8 months later the acetabulum looks almost round, while it looked flat before
In grade 3 the femoral head is found stable in a false acetabulum. This has a smaller sector of the weight bearing zone. But the sclerotic line became a bit longer after operation and almost horizontal. For a total hip later the conditions were improved too.
 This is the same grade 3 in a 16 year old girl. A shortening osteotomy had to be done to manage the rotation and the horizontal coverage. The weight bearing zone became indeed almost horizontal.
This is the same grade 3 in a 16 year old girl. A shortening osteotomy had to be done to manage the rotation and the horizontal coverage. The weight bearing zone became indeed almost horizontal.
Degrees |
Adolescents (% | Adults (%) |
|---|---|---|
1-4 |
n = 78 | n = 138 |
1. Fairly centered |
23.1 | 33.3 |
2. Femoral head dislocated in elongated acetabulum |
44.9 | 39.9 |
3. Femoral head in secondary acetabulum close to primary |
25.6 | 26.1 |
4. High secondary acetabulum |
6.4 | 0.7 |
Our hips in 26% had false acetabula and in 40-45% elongated acetabula. This has to be taken into consideration when dealing with this early material.
| Grade 0 | Painless hip |
|---|---|
| Grade 1 | Pain only at unusual and long exertions, no compromise of other activities |
| Grade 2 | Moderate pain, but limits ordinary activities to some degree |
| Grade 3 | Unremitting pain, marked limitation of activities |
| Grade 0 | No limitation |
|---|---|
| Grade 1 | Walking for more than 1 hour without pain |
| Grade 2 | Walking up to 1 hour possible |
| Grade 3 | Only short distances |
That was our clinical grading for pain and walking, similar to the Harris score. Patients opinion was added
| Very well | Well | Sufficient | Insufficient | |
|---|---|---|---|---|
Pain |
0 | 1 | 2 | 3 |
Walking |
0 | 1 | 2 | 3 |
Patients opinion |
1 | 2 | 2 | 3 |
Total |
1 | 2 - 4 | 5 - 6 | 7 - 9 |
| Grade | % |
|---|---|
Very good |
42.7 |
Good |
42.2 |
Fair |
12.3 |
Insufficient |
2.8 |
Tschauner combined all these things into one grading sytem. The results were: 42.7% very good and 42.2% good
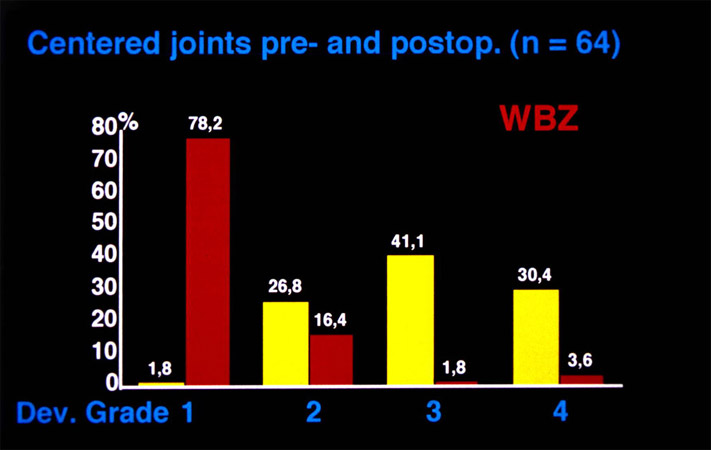
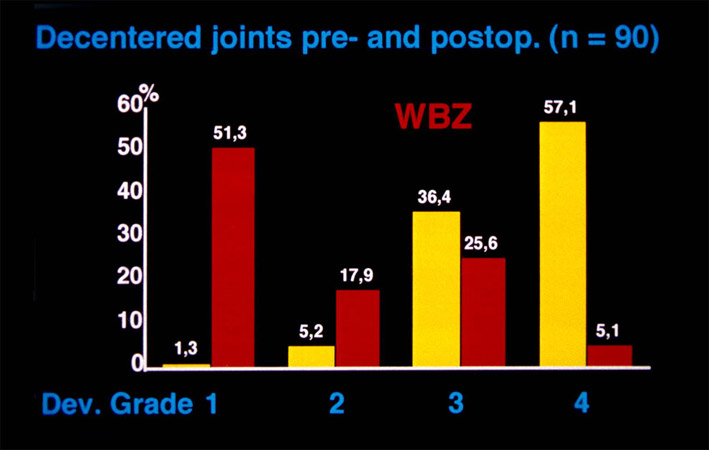
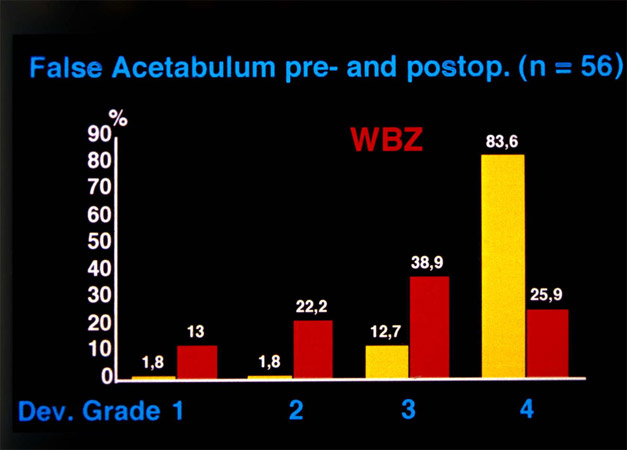
In these slides you find the correction of the weight bearing zone, the most important indicator of a normal hip. Our normal values and grades of deviation 1 to 4 are used here. Yellow - the preoperative value, - red the postoperative - at the left in the centered joints, at the right in the elongated acetabula. There, the preoperative values were much more pathological than in the centered joints. After operation, in the centered joints 78% had grade 1, in the decentered 51%. But this has changed later with more rotation of the tear drop figure.
In the false and high dislocated joints the deformation is even more accentuated before operation and showed less improvement postoperatively. But later this has improved as well.
| Grade | No pain (%) | Total (n) |
|---|---|---|
| 0 | 69.7 | 99 |
| 1 | 55.8 | 43 |
| 2 | 36.4 | 22 |
| 3 | 20.0 | 5 |
| Mose grade | No pain (%) | Total (n) |
|---|---|---|
| Normal (0 - 1) | 71.1 | 97 |
| Pathologisch (>1) | 45.3 | 69 |
There are, however, other factors, upon which we do have no influence: the degree of arthrosis of a joint, and the loss of sphericity of a femoral head which can be measured by the circles of Mose. Joints without arthrosis are free of pain in almost 70% and joints of Mose, grade only 1 and 2, are also free of pain in 71 %. Therefore treatment should begin when the patient feels regular pain on longer walking, not with the appearance of osteoarthrosis.
| 74,5% joints free of pain or with continuous improvement. |
| In 82% no increase of osteoarthrosis. |
| 9 hips (4%) received a total hip later. |
The results can be summarized as follows: 74.5% of the joints were free of pain or had a continuous improvement of pain. In 82% there was no increase of arthrosis. Secondary operations were rare. Only nine patients (4%) needed a total hip later when the deformations or the degree of arthrosis was too advanced.
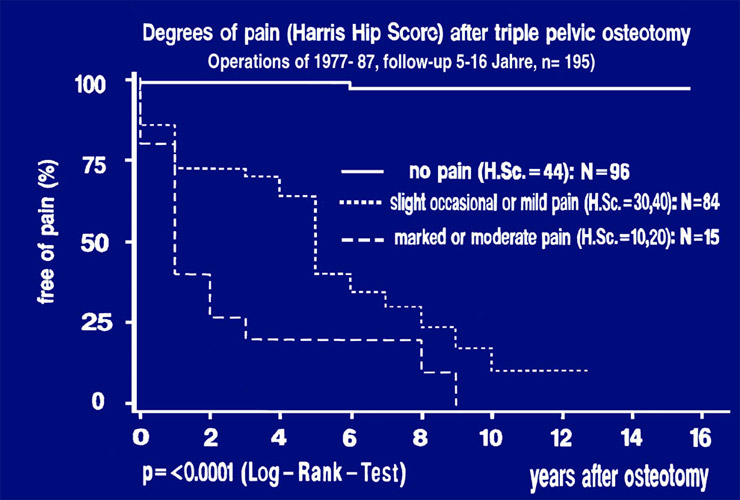 This is a survival rate curve out of the early material. Pain was classified after the Harris groups. No pain at all, the horizontal line on top, is the Harris group A. In the second curve from the top, the occasional and the mild pain of groups B and C are represented. In the lowest curve, with groups D and E, pain is severe and limiting function. 49% were free of pain in the Harris hip score, 43% had occasional and mild pain and 8% showed severe pain.
This is a survival rate curve out of the early material. Pain was classified after the Harris groups. No pain at all, the horizontal line on top, is the Harris group A. In the second curve from the top, the occasional and the mild pain of groups B and C are represented. In the lowest curve, with groups D and E, pain is severe and limiting function. 49% were free of pain in the Harris hip score, 43% had occasional and mild pain and 8% showed severe pain.
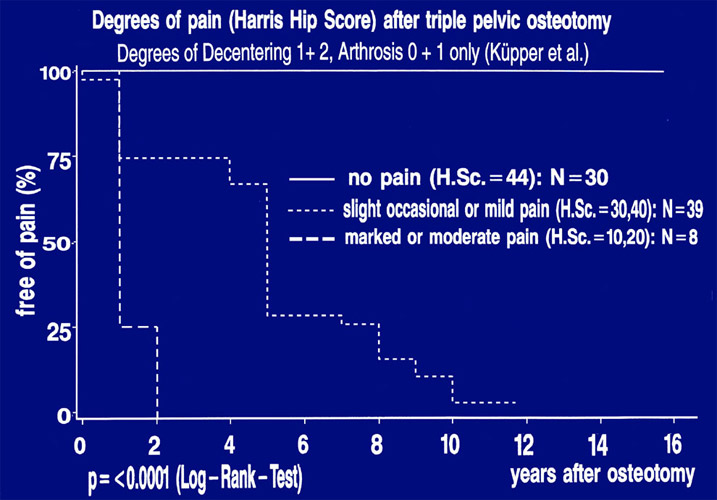 Let us now look at the new reinvestigation of Küpper. Here all patients operated in 1988 were followed up to 10 years when the degree of decentering was only 1 and 2, the degree of arthrosis 0 and 1, the classification of Mose 0 to 2. Therefore the number of joints was only 56. For the survival rate curve, we included joints of the opposite side when they were operated a short time earlier or later. The number of joints then came to 77. Here, 39% were free of pain, 51% had slight occasional or mild pain.
Let us now look at the new reinvestigation of Küpper. Here all patients operated in 1988 were followed up to 10 years when the degree of decentering was only 1 and 2, the degree of arthrosis 0 and 1, the classification of Mose 0 to 2. Therefore the number of joints was only 56. For the survival rate curve, we included joints of the opposite side when they were operated a short time earlier or later. The number of joints then came to 77. Here, 39% were free of pain, 51% had slight occasional or mild pain.
The 8 patients with severe pain (10%), I was astonished to see, that they had pain at the lower lumbar vertebras and the iliosacral joints. Their hip measurements were all normal. In total, I think, these are good results. The relatively large percentages of joints with mild or occasional pain are probably due to the decrease of anteversion up to negative values by anterior rotation of the acetabulum without internal compensating rotation. This had not been realized by us until the year 1998.
I want to add briefly the angle mesurements and the Harris score of the 10 years follow-up. The decisive angle of the weightbearing zone was found almost always in the normal range -10 to + 10° and the CE angle between 20 and 40°.
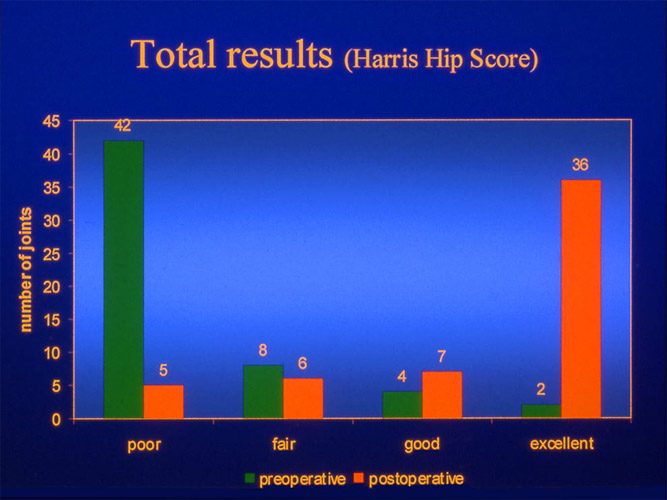 The total result of the Harris score was in 66% of the cases very good and in 14% good. This adds up to 80% ( 89 points ).
The total result of the Harris score was in 66% of the cases very good and in 14% good. This adds up to 80% ( 89 points ).
Complications of triple pelvic osteotomy
TPO |
188 |
|---|---|
TPO + FO |
63 |
Total |
251 |
| Localization | n | % | Total |
|---|---|---|---|
Os pubis |
8 |
||
Os ilium |
2 |
||
Pubis + Ilium |
1 |
||
Femur |
0 |
||
Total |
11 |
4.4 |
251 |
But complications have to be mentioned as well. Katthagen established a statistics of all 251 hips operated in 1999. It was differentiated between triple osteotomies exclusively and triple osteotomies combined with a femoral osteotomy. Pseudarthroses were found in only 4.4%, mainly at the pubis.
| Operation | n | % | Total |
|---|---|---|---|
TPO |
2 |
1.1 |
188 |
TPO + FO |
1 |
1.6 |
63 |
Total |
3 |
1.2 |
251 |
| Operation | n | % | Total |
|---|---|---|---|
TPO |
12 |
6.4 |
188 |
TPO + FO |
4 |
6.4 |
63 |
Total |
16 |
6.4 |
251 |
In total, embolism was noted in only 1.2%, thrombosis in 6.4%
| Sciatic nerve | n | % | Total |
|---|---|---|---|
| TPO | 4 | 2.1 | 188 |
| TPO + FO | 3 | 4.8 | 63 |
| Total | 7 | 2.8 | 251 |
Lesions of the sciatic nerve in triple osteotomy alone are listed with 2.1%, but with additional femoral osteotomy in 4.8%. This may be caused by a short longitudinal traction, movements or elongation of the leg. At the ischial osteotomy the nerve should be left covered by the muscles. Double curved retractors are safer than sharp edged. Also the tendon of the internal obturator muscle should remain dissected, since for the nerve it is a hypomochlion during flexion of the hip. Most of the lesions recovered to a great extent. Nevertheless, one has to be very careful.
| Peroneal palsy | 1.8% (4 in 220) |
|---|---|
| Obturator palsy | 1 (transitory) |
| Trendlenburg sign (increased) | 4 % (5 in 125) |
In the early follow-up we found only 1.8% of peroneal palsies. An increased Trendelenburg limp was found in 4%.
Indication and possibilities of triple pelvic osteotomy
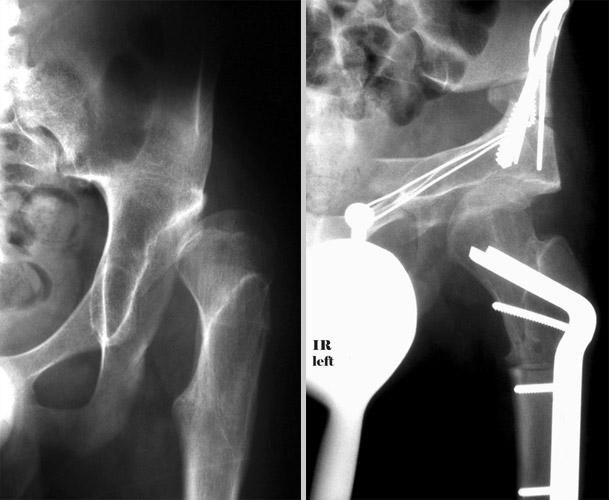
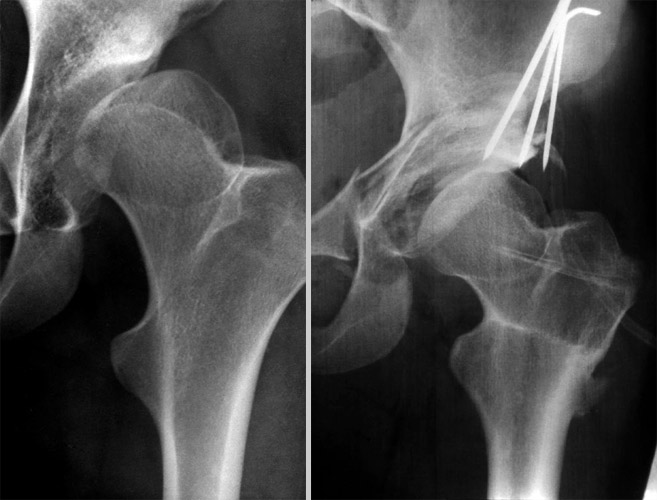
 In some pictures finely, I want to show you our indications and possibilities. This was a 24 year old patient, who had a Pemberton osteotomy in another country and an
extreme femoral anteversion. With our technique it was possible to cover the femoral head almost horizontally. The congruence inside the joint is not optimal. But sometimes there seem to be some adaptations.
In some pictures finely, I want to show you our indications and possibilities. This was a 24 year old patient, who had a Pemberton osteotomy in another country and an
extreme femoral anteversion. With our technique it was possible to cover the femoral head almost horizontally. The congruence inside the joint is not optimal. But sometimes there seem to be some adaptations.
 In the beginning, we left the dislocated joints in their lateralized position as seen here. But this means more load to the joint and stress to the muscles.
In the beginning, we left the dislocated joints in their lateralized position as seen here. But this means more load to the joint and stress to the muscles.

Therefore the next step can be seen in these two examples. We medialized the joints, and the functional results were further improved.

The acetabulum can be rotated extremely, when the ligaments of the sacrum are not fixing it any more, as you can see it here, but a varus-osteotomy had to be added in this case.
In high standing dislocations the femur has to be shortened when the acetabulum is turned down as far as to be seen in this case. This is mechanically necessary and the sciatic nerve would be stretched too much.

Here is a question of indication. Can you perform a triple osteotomy in this joint? The abduction, which we need for acetabular rotation, is blocked laterally by a bony edge. But the medial side of the femoral head is better rounded.
 This round part, which fits well into the acetabulum in adduction, we had to bring up by a valgus osteotomy of the femur combined with the lateral rotation of the acetabulum and there is a fair congruence now.
This round part, which fits well into the acetabulum in adduction, we had to bring up by a valgus osteotomy of the femur combined with the lateral rotation of the acetabulum and there is a fair congruence now.
The girl also had no femoral anteversion. This deformity should as well be noted and corrected to avoid further pain.
 This is an identical deformation. It is practically a method to turn the femoral head upright together with the acetabulum.
This is an identical deformation. It is practically a method to turn the femoral head upright together with the acetabulum.

Deformed femoral heads after Perthes disease can also be covered by triple osteotomy. When the greater trochanter is placed more lateral and distal, the femoral neck gets longer and as well the lever arm for the muscles.
 Here we have a similar situation in a 26 year old women. At the left, a flattened femoral head, only half covered, greater trochanter high and very close. At the right, the trochanter was transplanted lateral and distally. The femoral head then was congruently covered. Please compare the teardrop figures.
Here we have a similar situation in a 26 year old women. At the left, a flattened femoral head, only half covered, greater trochanter high and very close. At the right, the trochanter was transplanted lateral and distally. The femoral head then was congruently covered. Please compare the teardrop figures.
In this patient we used a varus osteotomy in addition to the lateral rotation of the acetabulum to cover the femoral head. We succeeded in the coverage, but the congruence inside the joint is only fair due to the deformed head. But for a total hip the conditions are better now.

Dysplasia of the hip in a 10 year old girl. Coxa valga. The pressure of the femoral head is directed against the lateral acetabular rim. Therefore the cartilagenous growth centers are developing an os acetabuli. Triple osteotomy covered the femoral head and centered the pressure into the acetabulum. The right picture shows the growth of the acetabulum after 5 years. Apparently the growth centers were relieved from pressure right in time.
My last pictures show the longest follow-up I have. They are from an airline-pilot whom I operated in 1982 at the age of 25. For 22 years and longer in the meantime he is now free of pain and presently working as captain of long range flights. His sports are Tennis, Golf and Mountainclimbing.
Dear colleagues, our triple osteotomy may look difficult, but the osteotomies are clearly visible and checked by the image intensifier. Everyone interested should visit us and learn it. My colleague, Dr. Kalchschmidt and others do 3-4 operations per week. Since 1976 we performed more than 5,000 osteotomies. The good 10 year results of the decentration grades 1 and 2, give us hope that these joints will not develop osteoarthrosis for a rather long time. When the anomalies of acetabular and femoral anteversion would be more diagnosed and corrected in the future, remissions of pain would be less.
| Download | |
|---|---|
| Triple Pelvic Osteotomy | PDF (1.2MB) |