Prof. Dr. med. Dietrich Tönnis
Sammlung wissenschaftlicher Arbeiten und Vorträge zur Orthopädie
Update of Triple Pelvic Osteotomy
Investigations performed at Orthopaedic Department of Klinikum Dortmund (Director B.-D. Katthagen, M.D.)
© Dietrich Tönnis, M.D.; Klaus Kalchschmidt, M.D.; Axel Küpper, M.D.; Achim Heinecke, Ph.D.; Bernd-Dietrich Katthagen, M.D.
By clicking on a figure an enlarged version of the figure will appear. At the end of the page you will find a PDF version of the paper.
ABSTRACT
Background: Our triple pelvic osteotomy has been performed 3626 times between 1976 and 2005. The technique was further elaborated. An update seems necessary.
Methods: The patient is now placed in a lateral supported position for the ischial osteotomy and then turned to supine position for the other osteotomies. The ischial osteotomy between sciatic notch and obturator foramen is necessary to separate the acetabulum from the sacrotuberal and sacroischial ligament for rotation. The ilium osteotomies are now performed from the inner side of the pelvis. Extreme lateral rotation of the acetabulum is possible when the lateral part of the pubis is pushed higher than the medial. Medialization to decrease the load of the joint is also possible then. Anterior rotation of the acetabulum is correctly when the Schanz screw lifts the acetabulum up posteriorly. Then the acetabulum keeps in contact with the long oblique osteotomized ischium. But, anterior rotation decreases acetabular anteversion. This has not been noted for a long time. The acetabulum has to be rotated internally to 15-20° in addition. When the anterior margin of the acetabulum overlaps the posterior, this demonstrates decreased acetabular anteversion. Reduced anteversion can also be present preoperatively in addition at femur and acetabulum and cause pain and impingement. Therefore the anterior coverage preoperatively can be controlled by the”false profil” radiography or a CT scan.
Material and Results: The results of 216 unselected joints reinvestigated after 5-16 years (mean 7.7) were good and very good in 85%, free of pain or with continuous improvement in 74.5%, no increase in osteoarthrosis in 82%. Another follow-up was performed after 11.5 years at 56 patients with decentration grades 1 and 2 only and osteoarthrosis grade 0 and 1, but of all osteotomies performed in 1988. The Harris hip score was good and excellent in 80%. The angle of the loading zone was normal in 52 of 56 joints (+ -10°), the CE angle 30-40° in 31.
Keywords: Update of triple pelvic osteotomy, present technique, results
INTRODUCTION
Acetabular rotational osteotomies have been used increasingly in the past years for redirection of dysplastic hip joints. A great number of modifications were described since LeCoer (1965) and Hopf (1966) described the first ones. They differ regarding the distance to the acetabulum and whether they release the acetabulum from the sacroischial ligaments or not. When the distance is too large, the rotation is very limited (Sutherland and Greenfield 1994). When ischium and ramus superior ossis pubis are osteotomized together, the teardrop figure and the onlying acetabular vessels will be cut (Eppright 1975, Hopf 1966). Osteonecrosis can follow.
The acetabulum can be rotated freely only when it is separated from the ischium with the sacrotuberal and sacrospinal ligament. That is included in our triple osteotomy (Fig. 1) and the periacetabular osteotomy of Ganz (Ganz et al. 1988). Carlioz (Carlioz et al.1982) does not separate the acetabulum completely by a transverse osteotomy of the ischium underneath the sacrospinal ligament. Steel (1973) osteotomized in front of the ischial tuberosity leaving both ligaments in place. The osteotomies of Ganz (1988), Carlioz (1982) and our hospital are the most used today. In our department 3.626 osteotomies have been performed between 1976 and 2005.
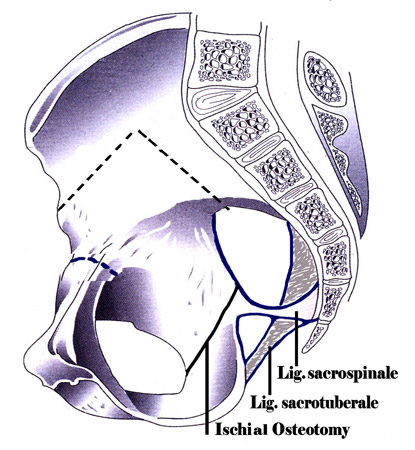 Fig. 1: Presentation of the three pelvic osteotomies. They allow a free rotation of the acetabular fragment by separating it from the ligaments of the sacrum. The plane of the ischial osteotomy can be seen properly only from the side and is not realistic here.
Fig. 1: Presentation of the three pelvic osteotomies. They allow a free rotation of the acetabular fragment by separating it from the ligaments of the sacrum. The plane of the ischial osteotomy can be seen properly only from the side and is not realistic here.
Since the first description (Tönnis et al. 1981) the technique has changed in different ways. Furtheron, the significance of decreased acetabular and femoral anteversion, either preoperatively already or postoperatively, concomitant with anterior rotation of the acetabulum, was not recognized by us before 1996 (Tönnis and Heinecke 1999, Tönnis and Skamel 2003). It is now treated additionally. An update of our technique is necessary.
METHODS
Measurements for control of acetabular rotation: Redirection of the acetabulum has to be performed in three planes. In the antero-posterior view the lateral rotation is controlled mainly by the angle of the weightbea-ring zone of Bombelli (Bombelli et al. 1984) and next the CE angle of Wiberg (1939). The lateral radiography was described by Lequesne and de Seze (1961) as the "false profil radiography". Here the patient is first standing lateral to the x-ray unit. The hip to be examined is positioned close to the x-ray film. The patient should then be rotated 25° towards the x-ray unit. The investigated hip this way is placed anteriorly to the other hip for a radiography from lateral. This angle was called VCA or anterior CE angle. Finally, the horizontal plane is controlled by computertomographies. They control the anteversion of the acetabulum and the femur (Tönnis and Heinecke 1999, Tönnis and Skamel 2003).
Early technique of triple pelvic osteotomy: We started with our technique in 1976. First we placed the patient into a prone position for the ischial osteotomy, which is easier for the beginning. Then he had to be turned into the supine position and draped again for the os ilium and os pubis osteotomy. The table is radiolucent.
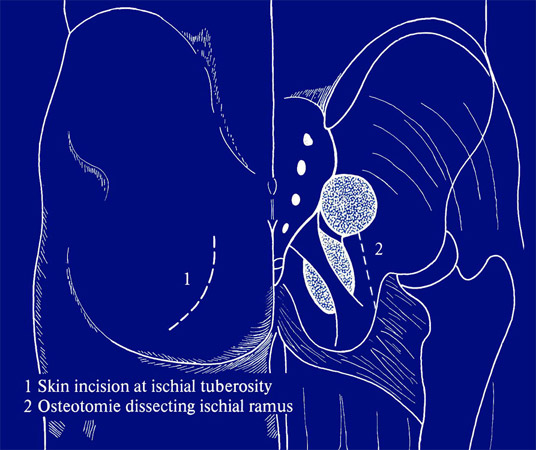 Fig. 2: Skin incision for the ischial osteotomy and the palpapel sacrotuberal ligament.
Fig. 2: Skin incision for the ischial osteotomy and the palpapel sacrotuberal ligament.
For the ischial osteotomy we palpate the ischial tuberosity and from there the sacrotuberal ligament (Fig. 2). An incision of 10 cm is made following the course of the ligament laterally. The fibers of the glutaeus maximus muscle are bluntly separated longitudinally to expose the ischial tuberosity and the sacro-tuberal ligament and the adjacent small external rotators (Fig. 3).
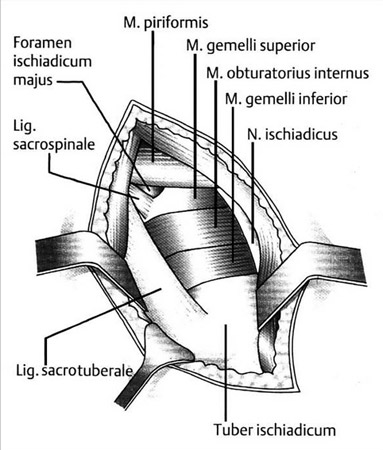 Fig. 3: Surgical exposure for osteotomy of the right ischium. Incision along the sacrotuberal ligament. The gluteus maximus fibers normally should cover the sciatic nerve, which is shown here for clarity. The fascia covering the small external rotators has already been removed.
Fig. 3: Surgical exposure for osteotomy of the right ischium. Incision along the sacrotuberal ligament. The gluteus maximus fibers normally should cover the sciatic nerve, which is shown here for clarity. The fascia covering the small external rotators has already been removed.
The sciatic nerve is shown laterally in the drawing, but we leave him covered by muscles during the operation. Every stronger pressure of retractors should be avoided. An incision is made at both sides of the sacrotuberal ligament. After perforating the membrane of the obturator foramen with a periostal elevator, a couple of long, specially shaped retractors are inserted. Proximally, the small external rotator muscles are covering the ischium. The tendons underneath of these muscles are cut. Then a small retractor is pushed beneath the muscles and placed into the sciatic notch lateral from the ischial spine, holding back these muscles (Fig. 4). One should not proceed more cranially where the neurovascular bundles are leaving the pelvic cavity. The whole posterior part of the ischium is now visible.
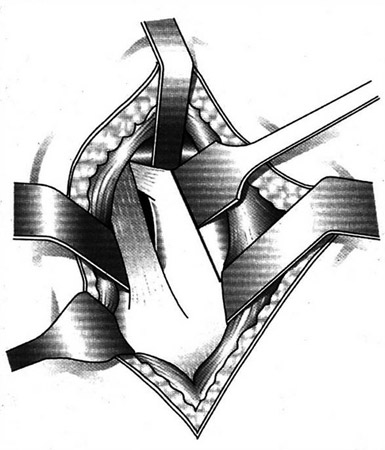 Fig. 4: The tendons underneath the rotators have been cut. A retractor inserted underneath of them and placed in the sciatic notch permits a good vision for the osteotomy.
Fig. 4: The tendons underneath the rotators have been cut. A retractor inserted underneath of them and placed in the sciatic notch permits a good vision for the osteotomy.
The ischial osteotomy between the sciatic notch and the obturator foramen should be long to guarantee consolidation later after anterior rotation of the acetabulum. The osteotomy should follow a line from the ischial spine to the midst of the ischial tuberosity. The osteotomy itself should be performed parallel, 1 cm anterior, not more. With a smaller chisel we start the osteotomy at the sciatic notch. Here the bone is relatively thin and the blade of the chisel can be palpated underneath and redirected before it approaches or enters the joint. A second broader chisel should then be directed parallel and towards the tips of the protecting retractors in the obturator foramen. As a rule, we say that the chisel should be directed 20° to 30° anteriorly from the frontal plane and towards the central longitudinal axis (Fig. 5).
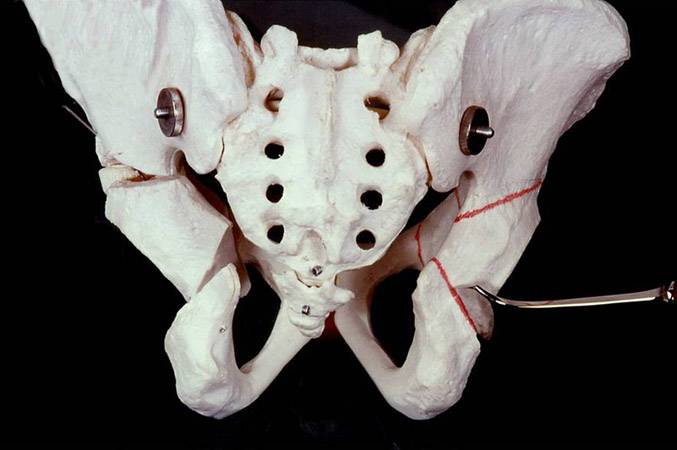 Fig. 5: This picture shows the direction of chiseling 20-30° anteriorly. The ischial osteotomy should be performed as long as possible, a bit more distally in the opturator formen (Fig. 1).
Fig. 5: This picture shows the direction of chiseling 20-30° anteriorly. The ischial osteotomy should be performed as long as possible, a bit more distally in the opturator formen (Fig. 1).
A chisel with less than 20° of anterior direction will run parallel to the obturator foramen. Rotation is not possible then. And with a direction of much more than 30° the chisel gets into the acetabulum. At the obturator foramen the chisel is directed to the tips of the retractors and to the lower circle of the foramen. The osteotomy has to be as long as possible for the acetabular rotation in the sagittal plane (Fig. 1). Afterwards we have to control whether the osteotomy is complete. The sharp inner bony rim of the obturator foramen is sometimes not osteotomized between the two retractors.
The easiest way to approach the pubis for the osteotomy is from the medial side, where it can be palpated underneath of the skin. One must take care not to proceed too far laterally. The femoral vein is lying laterally on the pectineus muscle. This muscle has to be released from the pubis to a great extend. Retractors underneath of the pubis have to protect the obturator artery. The periost we try to preserve for better healing. For the osteotomy we use a small oscillating saw with water cooling.
A third incision was now made along the iliac crest extending to the inguinal region. Under image intensified control, a Schanz screw was inserted not less than a centimeter above the acetabular roof medial-caudal parallel to the following inno- minate osteotomy, but directed 30-40° dorsally into the thicker part of the pelvis. The ilium osteotomy is now performed 2.5 cm above the Schanz screw (Fig. 6).
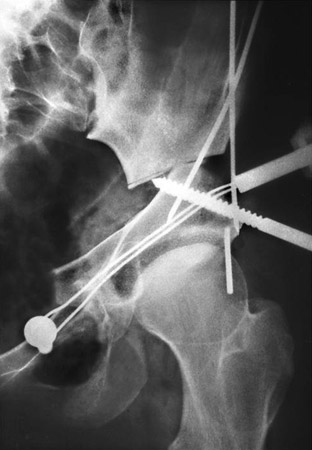 Fig. 6: The actabulum has been rotated by a Schanz screw with handle. The lateral end of the os pubis is placed above the medial. Provisional fixation with two K-wires, afterwards wire cerclage to stabilize the pubic osteotomy. A vertical short K-wire, as shown here, should be used to control anteversion.
Fig. 6: The actabulum has been rotated by a Schanz screw with handle. The lateral end of the os pubis is placed above the medial. Provisional fixation with two K-wires, afterwards wire cerclage to stabilize the pubic osteotomy. A vertical short K-wire, as shown here, should be used to control anteversion.
It is important that the osteotomy is descending and not horizontal, thereby allowing rotation of the acetabulum. Using the Schanz screw as a lever, the acetabulum can now be freely maneuvered in any direction.
At the same time, the acetabular ramus of the pubic ramus is pushed with the thumb upwards. In severe dysplasias this ramus is brought higher than the medial ramus and will overlap him, when we medialize the acetabulum for biomechanical reasons, especially to diminish its load (Fig. 7, 8). In these figures this is demonstrated. Also the osteosynthesis of the early time with Kirschner wires at the ilium and wire cerclages at the pubic osteotomy is shown here.
 Fig. 8: For an extensive acetabular rotation the
lateral part of the pubis after osteotomy has to be pushed above the medial part and then be medialized to diminish the load of the joint as seen here.
Fig. 8: For an extensive acetabular rotation the
lateral part of the pubis after osteotomy has to be pushed above the medial part and then be medialized to diminish the load of the joint as seen here.
A few words are necessary on the rotation of the acetabulum in 3 planes. Our goal is to bring the sclerotic line of the weight-bearing zone into a horizontal position (Fig. 9, 10). This is controlled by the image intensifier.
 Fig. 10: An extensive rotation laterally has been performed here as can be compared by
the position of the teardropfigure pre- and postoperatively. This patient was operated in
the beginning when we applied a plaster cast for 6 weeks after operation.
Fig. 10: An extensive rotation laterally has been performed here as can be compared by
the position of the teardropfigure pre- and postoperatively. This patient was operated in
the beginning when we applied a plaster cast for 6 weeks after operation.
In the second plane we have seen that there are frequently great deficits in the anterior coverage of the femoral head. Here, as well, the job is not done by only pulling the anterior part of the acetabulum distally. As the drawing in Fig. 11 shows we have to turn the posterior part of the acetabulum upwards with the Schanz screw and rotate it in total. Its lower part has to glide upwards on the plane of the osteotomy (Fig. 12-13).
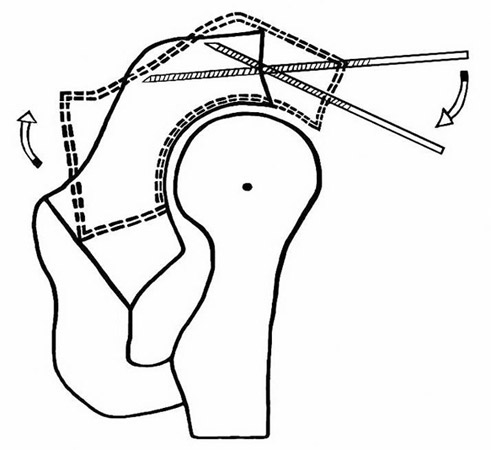 Fig. 11: Technique of the anterior rotation of the acetabulum by pushing the tip of the Schanz screw upwards posteriorly. The acetabular fragment has to glide upwards on the plane of the ischium osteotomy and remain in contact for fusion later.
Fig. 11: Technique of the anterior rotation of the acetabulum by pushing the tip of the Schanz screw upwards posteriorly. The acetabular fragment has to glide upwards on the plane of the ischium osteotomy and remain in contact for fusion later.
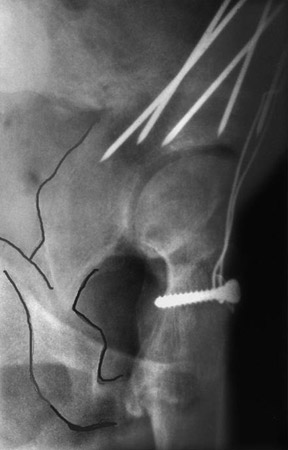 Fig. 13: The acetabulum has been rotated as shown in Fig. 11. The coverage of the femoral head is improved. The fusion at the ischial osteotomy is progressing.
Fig. 13: The acetabulum has been rotated as shown in Fig. 11. The coverage of the femoral head is improved. The fusion at the ischial osteotomy is progressing.
If there is a higher dislocation of the femoral head and a larger deficit of the anterior coverage, we have to bring another Schanz screw into the acetabular roof from anterior to rotate the posterior part of the acetabulum anteriorly. Fig. 14 shows a picture how it should not be done. Only the upper part of the acetabulum is inclined and levered down anteriorly, and the posterior lower margin has not moved upwards on the osteotomy plane. Now there is a big gap in the ilium osteotomy and pseudarthroses may develop.
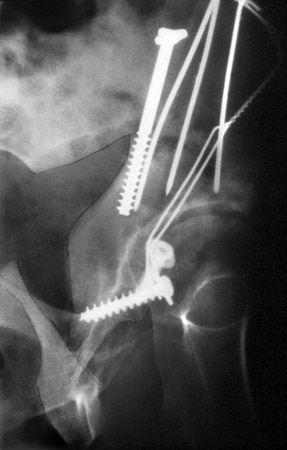 Fig. 14: Anterior rotation of the acetabulum as it should not be done. It is tilted and levered forward and distally from a point at the lower end of the ischial osteotomy. The rotatation is not sufficient then and pseudarthroses may develop in the ilium osteotomy causd by the bigger gap here.
Fig. 14: Anterior rotation of the acetabulum as it should not be done. It is tilted and levered forward and distally from a point at the lower end of the ischial osteotomy. The rotatation is not sufficient then and pseudarthroses may develop in the ilium osteotomy causd by the bigger gap here.
Present technique of triple pelvic osteotomy: The patient is now placed in a lateral supported position for the ischial osteotomy and can be turned then without further draping into the supine position for the pubic and ilium osteotomy. The table is radiolucent.
The upper pubis osteotomy is now medially inclined and also dorsally directed (Fig. 15). This allows a medial shifting of the acetabulum, and additionally the acetabulum can be better rotated around the vertical axis for anomalies of the anteversion and after anterior rotation of the acetabulum.
 Fig. 15: The pubic osteotomy is now inclined medialy for shifting the acetabulum medially, and also dorsally for rotation around the vertical axis.
Fig. 15: The pubic osteotomy is now inclined medialy for shifting the acetabulum medially, and also dorsally for rotation around the vertical axis.
The ilium osteotomy Kalchschmidt performs now similar to the technique of Millis (Millis and Murphy 1998) from the inner side of the pelvis by an anterior approach which is "abductor sparing". First, the anterior superior iliac spine with the attached sartorius muscle and inguinal ligament origins is detached in the thickness of a centimeter to facilitate the anterior approach. Then, the iliacus muscle is released from the pelvic wing. Under image intensifier control and maximal abduction of the leg, a 5 mm Schanz screw with a handle for acetabular rotation is inserted from lateral above the center of the femoral head and 30°-40° directed posteriorly, and not less than a centimeter above the acetabular roof. The osteotomy is performed 2.5 centimeters above the Schanz screw to give hold for 2-3 cancellous bone screws coming from the iliac crest and os pubis.
The osteotomy begins at the sciatic notch aiming to a point on the iliac crest 5 cm dorsal to the anterior superior iliac spine (Fig. 16). But 3-4 cm before, the osteotomy is directed distally by an angle of almost 90°. The advantage is that there is no bigger gap after anterior rotation, which would require bone chips. The osteotomy should laterally be ascending proximally. Otherwise the acetabular rotation would be impeded.
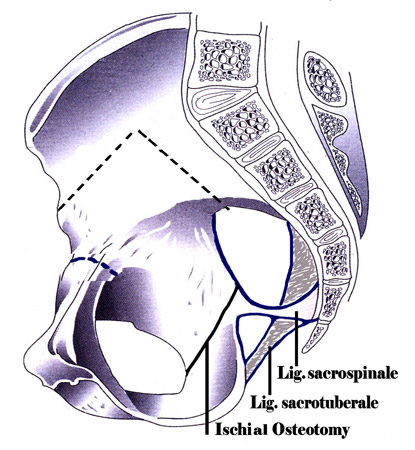 Fig. 16: New type of ilium osteotomy performed from the inner side of the pelvis by an anterior approach.
Fig. 16: New type of ilium osteotomy performed from the inner side of the pelvis by an anterior approach.
The ilium osteotomy is first marked with a chisel. For the hard bone around the sciatic notch, we prefer a Tuke saw which is not traumatizing soft tissue adjacent to the bone. In the sciatic notch a longer and broader retractor is protecting the sciatic nerve.
In some patients with longer existing pain the adductor muscles are shortened and the capsule has shrinked. Lateral rotation of the acetabulum in these patients is limited. Then the capsule medially has to be incised and also the origin of the adductors.
The third plane of the hip joint, the horizontal, has so far found very little interest in Orthopaedics. We also have not realized its significance in the beginning. Later we found that decreased acetabular and femoral anteversion can also cause pain, impingement and osteoarthrosis and especially if both have severely deceased angles. (Tönnis and Heinecke, 1999, Tönnis and Skamel, 2003).
In Fig. 17 the anteversion angle is decreased close to zero at the right joint and to 6 degrees at the left. At the same time the femoral anteversion was decreased. In this horizontal plane we have to rotate the acetabulum and the femoral neck to a normal anteversion of 15° to 20°.
 Fig. 17: Pelvis with decreased acetabular anteversion, at the right close to zero, at the left to - 6°. The measurement has to be taken at a level where the anterior acetabular rim is still long and congruent. Here the impingement takes place. At lower levels of the tomogramm the anterior rim is drawing back and disappears. This CT has to be taken in prone position (28, 29, 30).
Fig. 17: Pelvis with decreased acetabular anteversion, at the right close to zero, at the left to - 6°. The measurement has to be taken at a level where the anterior acetabular rim is still long and congruent. Here the impingement takes place. At lower levels of the tomogramm the anterior rim is drawing back and disappears. This CT has to be taken in prone position (28, 29, 30).
But there is still another problem in this plane. We noticed for a long time, that the internal rotation of the hip was decreased to some degree after triple osteotomy. So we tried to rotate the acetabulum a bit internally when we fixed it. Then we found the papers of Visser and Jonkers (1980) and of Anda et al. (1990).
In Fig. 19 compared to Fig. 18 the model of the pelvis is inclined anteriorly and the anterior margin now has moved more laterally. This way acetabular anteversion is decreased to zero. With lateral rotation of the whole pelvis (Fig. 20) during radiography or of the acetabulum at operation, anteversion is also completely diminished.
 Fig. 18: Model of a pelvis in an almost normal anterior inclination (tilt). Here the acetabular cavity is partially seen because the anterior acetabular rim is situated more medially than the posterior, and in the midst of the joint the distance has its maximum.
Fig. 18: Model of a pelvis in an almost normal anterior inclination (tilt). Here the acetabular cavity is partially seen because the anterior acetabular rim is situated more medially than the posterior, and in the midst of the joint the distance has its maximum.
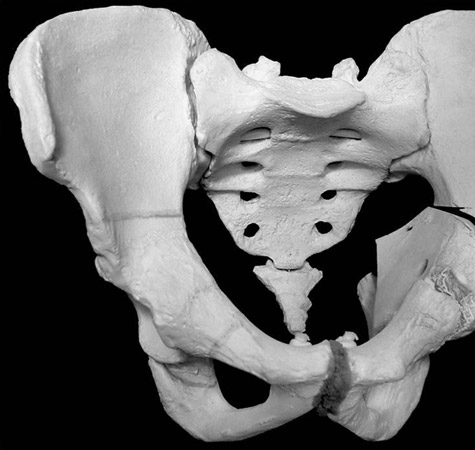 Fig. 19: With increased pelvic inclination or anterior rotation of the acetabulum the distance of the two rims disappears. Anteversion comes to zero. Therefore an additional internal rotation of the acetabulum is necessary after anterior rotations until the rims are seen separately as normal.
Fig. 19: With increased pelvic inclination or anterior rotation of the acetabulum the distance of the two rims disappears. Anteversion comes to zero. Therefore an additional internal rotation of the acetabulum is necessary after anterior rotations until the rims are seen separately as normal.
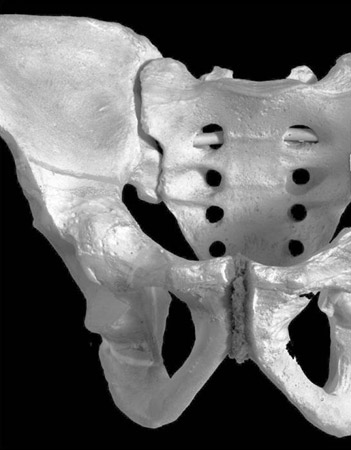 Fig. 20: With lateral rotation of the pelvis during radiography or of the acetabulum at operation, anteversion is also decreased to zero or retrotorsion.
Fig. 20: With lateral rotation of the pelvis during radiography or of the acetabulum at operation, anteversion is also decreased to zero or retrotorsion.
In Fig. 21 preoperatively, the acetabular anteversion is somewhat decreased; the anterior margin overlaps the posterior only laterally to some degree. This should have been corrected. But after triple osteotomy (Fig. 22) the anterior margin has descended extremely almost to the midst of the femoral head.
 Fig. 21: In this 26 years old patient with an os acetabuli at the lateral acetabular rim, acetabular anteversion is already decreased as the anterior acetabular rim crosses the posterior rim laterally.
Fig. 21: In this 26 years old patient with an os acetabuli at the lateral acetabular rim, acetabular anteversion is already decreased as the anterior acetabular rim crosses the posterior rim laterally.
 Fig. 22: After triple osteotomy the anterior acetabular rim has decended extremely to the midst of the femoral head. Acetabular anteversion was further diminished.
Fig. 22: After triple osteotomy the anterior acetabular rim has decended extremely to the midst of the femoral head. Acetabular anteversion was further diminished.
Some surgeons believe that this shows a good ventral coverage. But the acetabulum should have been rotated internally until the anterior and the posterior margin show a normal distance. The ventral coverage we control by the lateral faux profil radiography (Fig. 12-13).
The lateral radiographies of the next patient (Fig. 23-24) pre- and postoperatively prove that only a moderate anterior rotation was performed up to the point where the lower margin of the femoral head and the acetabulum were standing at the same hight, the limit of anterior rotation.
 Fig. 23: The faux-profil lateral radiography preoperatively shows that the lower margin of the femoral head is standing higher than the lower rim of the acetabulum, but in a moderate distance.
Fig. 23: The faux-profil lateral radiography preoperatively shows that the lower margin of the femoral head is standing higher than the lower rim of the acetabulum, but in a moderate distance.
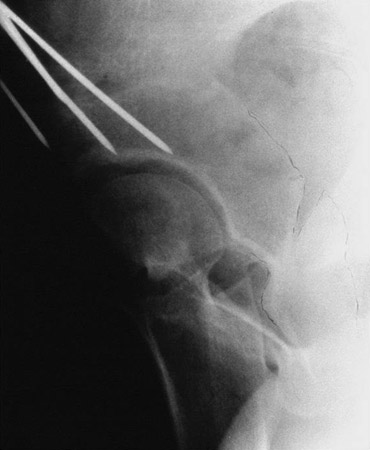 Fig. 24: The acetabulum was rotated anteriorly. The lower rim of the acetabulum has been moved up to the lower margin of the femoral head, the limit. This is a moderate anterior rotation and not as excessive as to decend anteriorly to almost the midst of the femur.
Fig. 24: The acetabulum was rotated anteriorly. The lower rim of the acetabulum has been moved up to the lower margin of the femoral head, the limit. This is a moderate anterior rotation and not as excessive as to decend anteriorly to almost the midst of the femur.
In the preoperative picture the os acetabuli is seen at the top of the femoral head; postoperatively it comes to an anterior VCA angle of about 25°. This is a lower borderline. However, the ap view postoperatively showed the anterior acetabular margin near the center of the femoral head. This shows only the decrease of acetabular anteversion. It is the result of a retroverted acetabulum and should not be correlated with the VCA angle. This deep anterior margin is caused by each anterior rotation. Some colleagues think that this shows a good anterior coverage and rotate the acetabulum laterally to retroversion. Before acetabular rotation starts we recommend to put a short, in the supine position of the patient a vertical K-wire, into the acetabular roof to maintain control (Fig. 6).
After lateral and anterior rotation one should always rotate the acetabulum internally to a normal anteversion (15°-20°) with separate anterior and posterior acetabular margins. After a primary fixation this has to be proved by a normal internal rotation of the hip at 45° of flexion. It should not be decreased.
In the beginning we performed the fixation of the ilium-osteotomy with 3 mm Kirschner-wires and applied a plaster cast for 6 weeks. Then we used 2 or 3 screws and fixed the osteotomy of the pubis with a cerclage. At present Kalchschmidt uses 6.5 mm cancellous bone screws for the ilium . First, a screw with a short screw-thread is used to pull the acetabular fragment against the ilium. Then, one or two screws with a long screw-thread are keeping the osteotomy in this position with pressure. Thereafter, the first screw is changed also to a long screw-thread. If possible screws are used also for the pubis-osteotomy (Fig. 25).
In small pubic bones a 4.0 mm screw is used. This thinner screw break in a small number, may be 10% in the last 5 years during daily life or at the removal, the 6.5 mm screw very rarely. However, the proximal part can be left in the pelvis without problems.
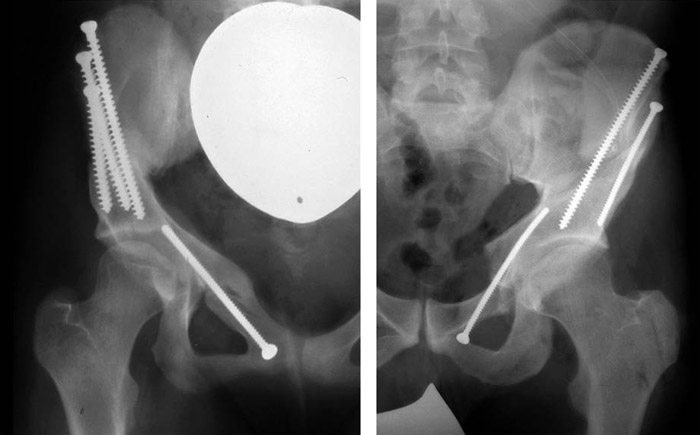 Fig. 25: New technique for the osteosynthesis of the pubis osteotomy with screws.
Fig. 25: New technique for the osteosynthesis of the pubis osteotomy with screws.
Treatment after operation: After operation the peridural catheter that had been used for anesthesia is left in place for 2-3 days more to diminish pain postoperatively. After 4 to 5 days patients can walk on crutches without weight bearing. After 12 to 14 days they are sent home. Ad- and abduction of more than 30° should be avoided in the first weeks, also external rotation. The hip can be flexed up to 60°. Internal rotation should be exercised to train the abductor muscles. A radiological control is advised after 6 and 12 weeks. According to the consolidation of the osteotomies partial and later full weight bearing can be allowed.
MATERIAL
Reinvestigations were performed at different times. The first longer follow-up contained the unselected early material operated between 1977 and 1987 and reinvestigated between 5 and 16 years, mean 7.7 years (Tönnis et al. 1994). 351 patients with 393 joints were operated. 197 patients with 216 joints could be reinvestigated. One woman had died because of embolism a short time after operation. 153 had changed their address and could not be found. 78 operations had been performed on children and adolescents and 138 on adults. 14.6% of the patients were male, 85.2% female. In 58.3% the left hip was operated, in 41.7% the right.
The deformations of the joints were quite different. Therefore we introduced four grades of decentration. In grade 1 the joint is fairly centered and spherical and best results can be expected (Fig. 45). In grade 2 the femoral head is dislocated in an elongated acetabulum, but can be recentered with a good rotation (Fig. 7-8). In grade 3 the femoral head is found stable in a false acetabulum (Fig. 26-27).
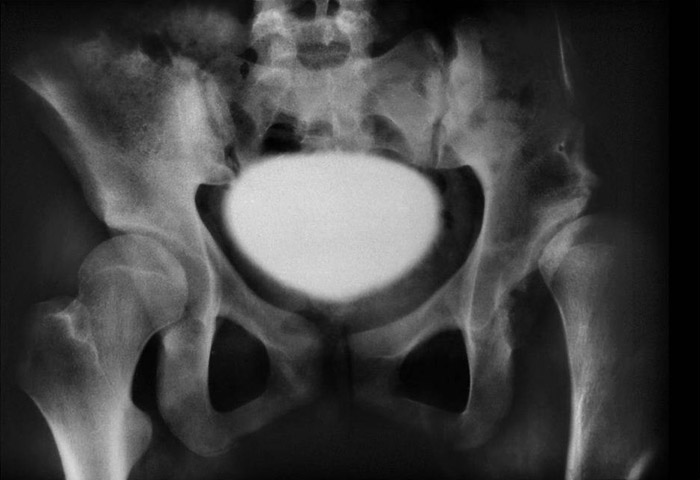 Fig. 26: Hip joint of decentering grade 3, a false acetabulum, in a girl 16 years of age.
Fig. 26: Hip joint of decentering grade 3, a false acetabulum, in a girl 16 years of age.
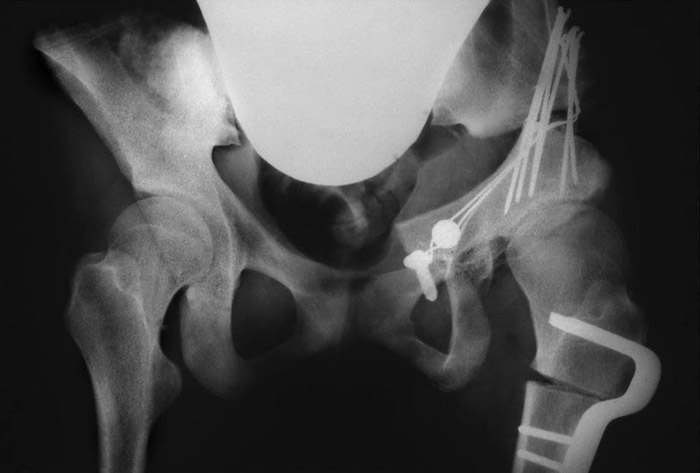 Fig. 27. A triple pelvic osteotomy was performed and a shortening osteotomy of the femur before, to avoid a stretching trauma to the sciatic nerve. A fair coverage with an excessive medialisation of the joint was achieved. The
weightbearing area in a false joint however is smaller than in a normal.
Fig. 27. A triple pelvic osteotomy was performed and a shortening osteotomy of the femur before, to avoid a stretching trauma to the sciatic nerve. A fair coverage with an excessive medialisation of the joint was achieved. The
weightbearing area in a false joint however is smaller than in a normal.
This has a smaller sector of the weight bearing zone. In grade 4 the femoral head is highly dislocated. but it can be reduced by abduction. Our hips in 26% had false acetabuli and in 40/45% (adults/adolescents) elongated acetabuli. High dislocations were found in 7%. This has to be taken into consideration when dealing with this early material.
Position of the acetabulum: At the operation and at the evaluation of the results the question arises: which is the best position for the acetabulum? Our answer is: the best angle causes no pain. We evaluated this fact at the early reexamination (Tönnis et al. 1994). Tab.1 shows the angles with the highest percentage of joints without pain. For each angle the 95% confidence intervals for the percentages of joints without pain were computed and compared with the 95% confidence interval for the greatest percentage. Thus we found significant differences (no overlapping) and tendency of difference (mild overlap-ping) between these percentages. It was interesting to see that the borderlines of other authors appeared here as well to some extent.
| VCA angle | 30 - 35° |
|---|---|
| CE angle | 30 - 35° |
| Loading zone angle | -5 to +5° |
| Migration (%) | 10 - 15 |
The CE-angle of Wiberg (1939) had its maximum of 78.1% joints free of pain at an angle of 30°-35°. The 95% confidence interval was found for the angle group <10° (the severes dysplasias) and a tendency of difference to the group 10°-20° (the moderate dysplasias). Wiberg and later Severin (1941) considered angles larger than 25° as normal. Severin did not count angles from 20°-<25°. And only those beneath 20° were taken as pathological.
For the anterior VCA angle of Lequesne and de Seze (1941) the findings were quite similar.
The angle of the weight bearing zone had its maximum of joints free of pain at -5° to + 5°. Lingg and v.Torklus (1981) investigated this angle already 1967 and considered angles between –9,6° to +9,3° as normal. We found the 95% confidence interval at angle group 11°-15°. This coincides with the +9.3° upper borderline of Lingg and v. Torklus. The normal area can be considered as –10° to +10°. Our <-5° group, with 6 joints, was too small for investigation. The –5° to +5° angle has to be considered as the optimal angle group, as it are 30° to 35° in relation to 25° to 29° in the CE angles.
The migration percentage of Reimers (1980) describes which percentage of the femoral head diameter is not covered or too much. The optimum was found at 10-15% uncoverage. Astonishing is that the 95% confidence interval was present already to the next higher and lower percentage group. 10-15% are normal, but less and 5% more are already critical. The further groups of uncoverage have also a 95% confidence interval (25 to <35%) or tendencies (20 -<25% and >35%). That depends on the number of joints too.
This is the same, regarding the other values: at overcorrection pain is increasing. So we found optimal values and values of overcorrection (Tab. 2). For the evaluation of results we defined normal values and grades of deviation: mildly, severely and extremely pathological (Tab. 3). Overcorrection should be avoided as well.
| CE angle | > 40° |
|---|---|
| VCA angle | > 40° |
| Loading zone angle | < - 10° |
| Migration (%) | < 10° |
| Degrees | 1 (normal) |
2 (mildly pathological) |
3 (severely pathological) |
4 (extremely pathological) |
|---|---|---|---|---|
| CE angle | ≥ 30 |
20 - 29 |
5 -19 |
< 5 |
| VCA angle | ≥ 25 |
20 - 24 |
5 - 19 |
< 5 |
| Load. zone angle | ≤ 9 |
10 - 15 |
16 - 25 |
> 25 |
| Reimers ind. | ≤ 15 |
16 - 25 |
26 - 40 |
> 40 |
| Hip Value | < 16 |
16 - < 21 |
21 - < 31 |
≥ 31 |
RESULTS
Our clinical grading for pain and walking, similar to the Harris score, is shown in Tab. 4 and 5. Patients’ opinion was added.
| Grade 0 | Painless hip |
|---|---|
| Grade 1 | Pain only at unusual and long exertions, no compromize of other activities |
| Grade 2 | Moderate pain, but limits ordinary activities to some degree |
| Grade 3 | Unremitted pain, marked limitation of activities |
Grade 0 |
No limitation |
|---|---|
Grade 1 |
Walking for more than 1 hour without pain |
Grade 2 |
Walking up to 1 hour possible |
Grade 3 |
Only short distances |
Tschauner et al. (1998) combined all these criteria into one grading system (Tab. 6). The results were: 42% very good, and 42% good (Tab. 7).
| very well | well | sufficient | not sufficient | |
|---|---|---|---|---|
| Pain | 0 |
1 |
2 |
3 |
| Walking | 0 |
1 |
2 |
3 |
| Patients' opinion | 1 |
2 |
2 |
3 |
| Total | 1 |
2-4 |
5-6 |
7-9 |
| Grade | % |
|---|---|
very good |
42,7 |
good |
42,2 |
fair |
12,3 |
insufficient |
2,8 |
The quality of acetabular redirection is shown in Fig. 28-31 by control of our normal values and grades of deviation up to 4 (Tab. 3). After operation, in the centered joints, 78% had grade 1, in the decentered 51%. In the false and high dislocated joints the deformation was even more accentuated before operation and showed less improvement postoperatively.
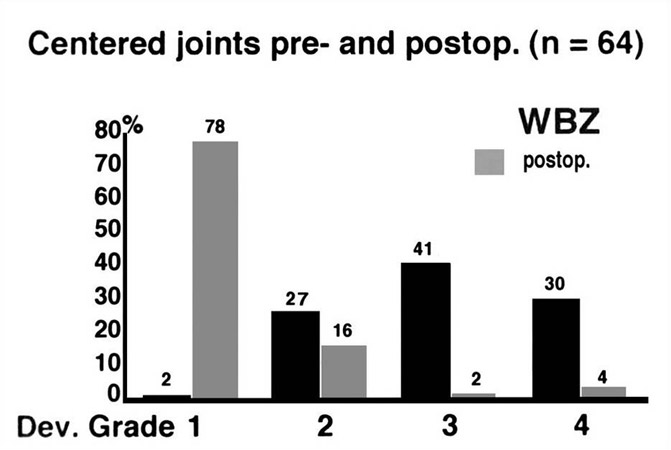 Fig. 28: Centered joints pre- and postoperatively (n=64)
Fig. 28: Centered joints pre- and postoperatively (n=64)
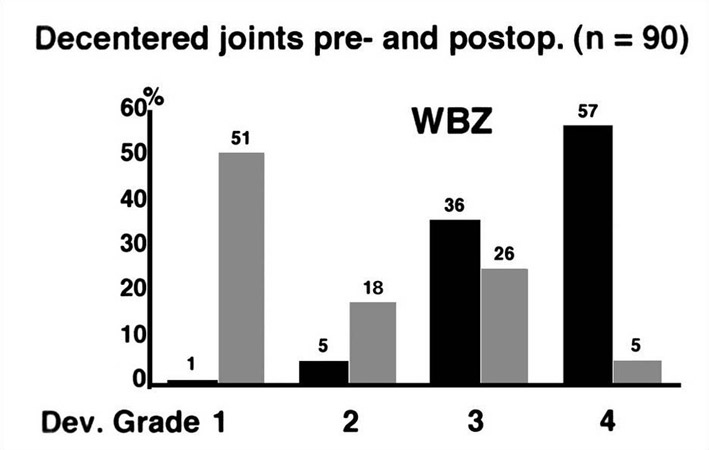 Fig. 29: Decentered joints pre- and postoperatively (n=90)
Fig. 29: Decentered joints pre- and postoperatively (n=90)
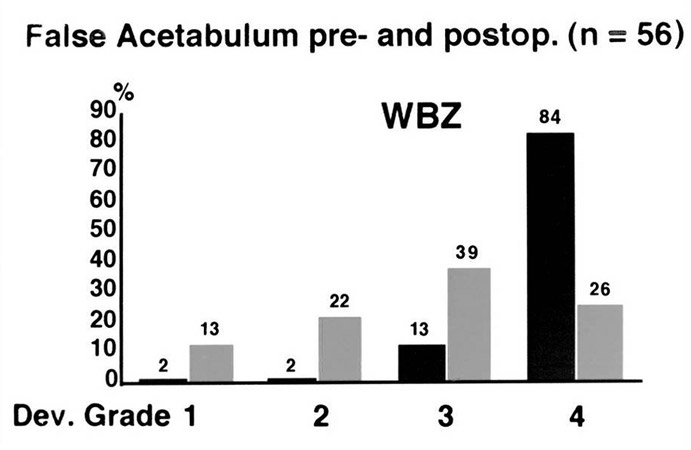 Fig. 30: False acetabuli pre- and postoperatively (n=56)
Fig. 30: False acetabuli pre- and postoperatively (n=56)
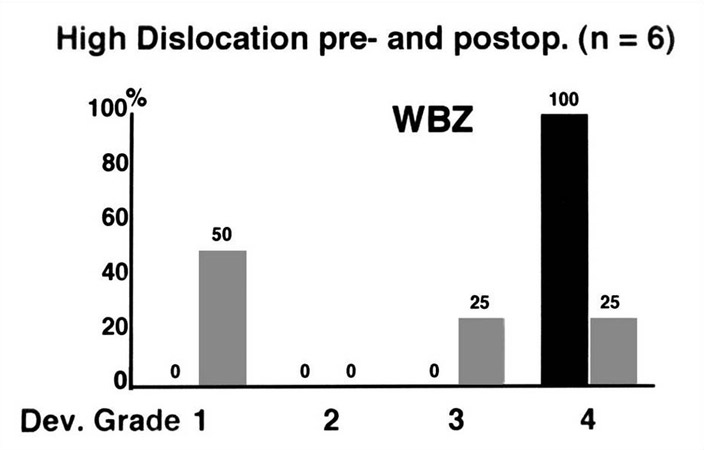 Fig. 31: High dislocations pre- and postoperatvely (n= 6)
Fig. 31: High dislocations pre- and postoperatvely (n= 6)
The results can be summarized as follows: 74.5% of 216 joints were free of pain or had a continuous improvement of pain. In 82% of 213 there was no increase of arthrosis. Secondary operations were rare. Only nine patients (4%) needed a total hip later when the deformations or the degree of arthrosis was too advanced.
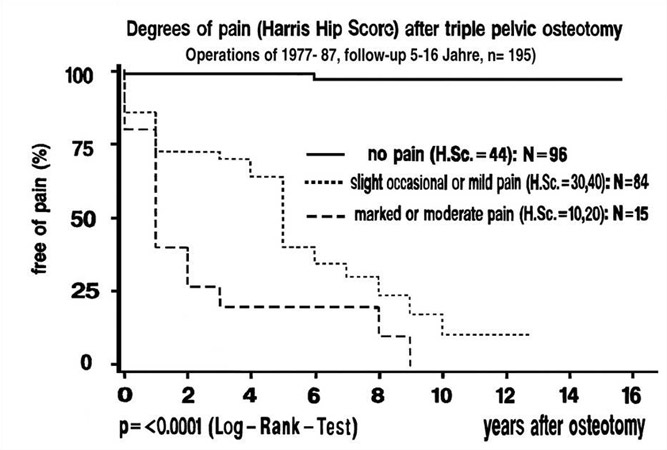
Fig. 32 shows a survival rate curve out of the early material. Pain was classified after the Harris groups (Harris 1969). No pain at all, the horizontal line on top, is the Harris group A. In the second curve from the top, the occasional and the mild pain of groups B and C are represented. In the lowest curve, with groups D and E, pain is severe and limiting function. 49% were free of pain in the Harris hip score, 43% had occasional and mild pain and 8% showed severe pain.
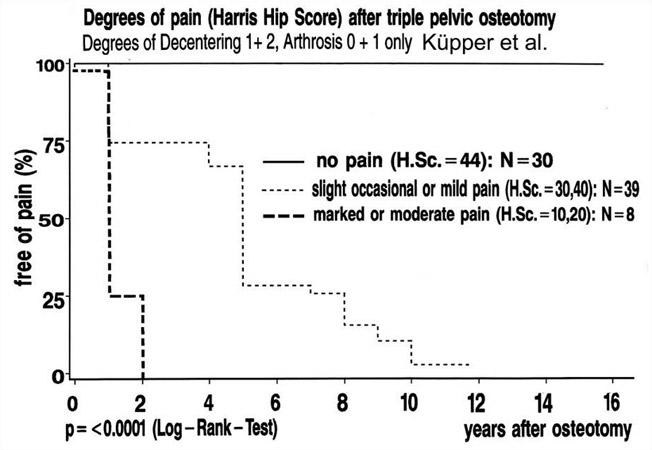
Second follow-up of selected material: A 11.5 year follow-up was presented by Küpper (2002). All patients operated in 1988 who´s hip joints had a degree of decentration 1 or 2 and a degree of arthrosis 0 or 1 and degrees of Mose 0 to 2 were included. Patients with previous surgery and joints with a simultaneous intertrochanteric osteotomy were excluded. Overall 55 patients were included in the study. Follow-up was obtained in 54 patients with 56 operated hip joints.
The Harris hip score (Fig. 33) improved from an avarage of 60.6 points preoperatively to an avarage of 89.3 points at follow-up. Preoperatively the score was poor or fair in 89.3%, at the latest follow-up the score was excellent and good in 80.4%. Radiographs with a follow-up of at least 10 years were available in 51 cases (94%). Before Triple Osteotomy a degree of decentering 1 was seen in 54%, a degree 2 in 46%. 51 joints (91%) showed preoperatively no osteoarthrotic changes; five joints (9%) were in the early stage of degree 1 of arthrosis. At an avarage radiographic follow-up of 11.2 years, 50 hip joints (89%) showed no signs of osteoarthrosis. In 2 cases of grade 1 the findings were unchanged. In 4 hips (2 patients) the severity of osteoarthrosis had increased. One of these patients needed a total hip arthroplasty.
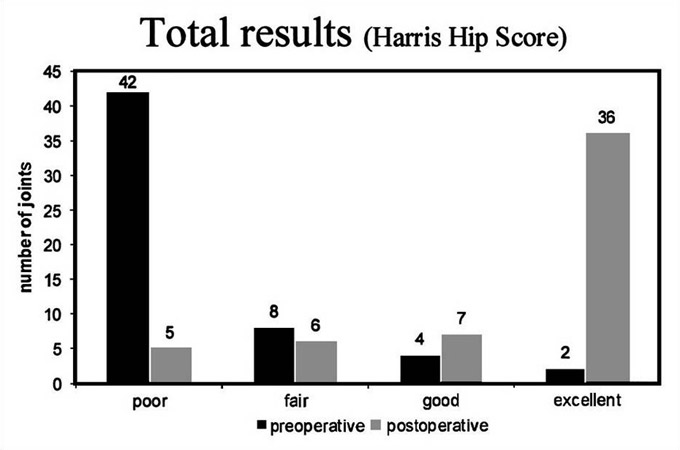 Fig. 33: Total results (Harris hip score), pre- and postoperatively
Fig. 33: Total results (Harris hip score), pre- and postoperatively
The most important acetabular angles pre- and postoperatively are shown in Fig. 34 and 35. The weight bearing zone (Bombelli et al. 1984) was found nearly always in the normal range –10° to +10° (average 0.2°, SD 6.0°) and the lateral CE angle between 20 and 40 degrees (avarage of 33.5°, SD 6.9), the anterior CE angle at an avarage of 34.8°, SD 8.6°.
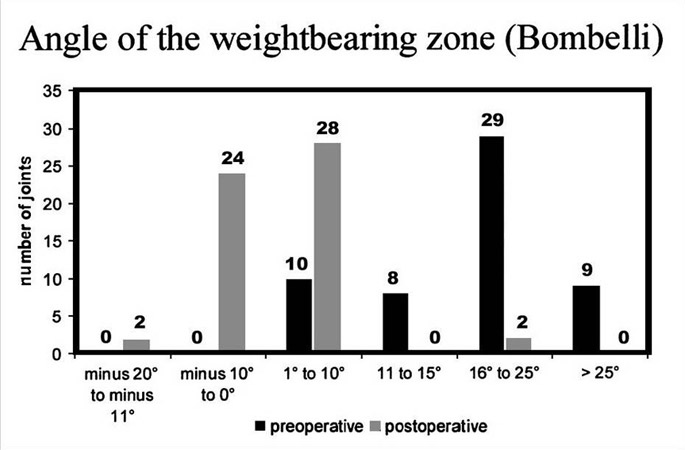 Fig. 34: Angle of the weight bearing zone (Bombelli) pre- and postoperatively
Fig. 34: Angle of the weight bearing zone (Bombelli) pre- and postoperatively
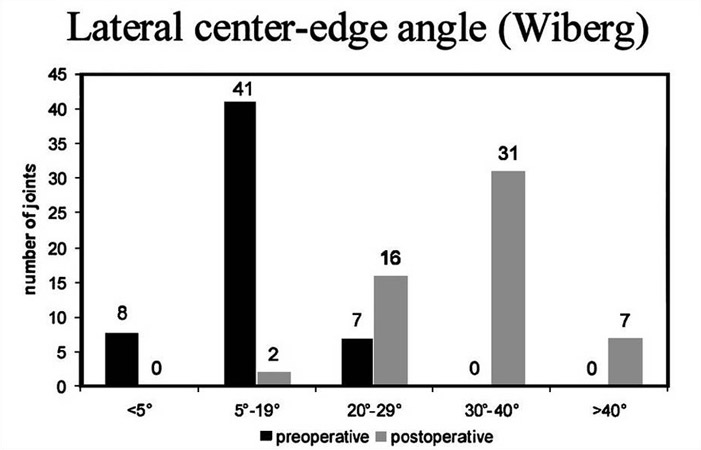 Fig. 35: Lateral center edge angle (‘Wiberg’) pre- and postoperatively
Fig. 35: Lateral center edge angle (‘Wiberg’) pre- and postoperatively
For a survival rate curve (Fig. 36), we included joints of the opposite side when they were operated a short time earlier or later. The number of joints then came to 77. Here, 39% were free of pain, 51% had slight occasional or mild pain and 8 patients severe pain (10%), but mainly at the lower lumbar vertebras and the iliosacral joints. Their hip measurements were all normal.
Complications: Complications have to be mentioned as well. Katthagen et al. (2001) established a statistics of all 251 hips operated in 1999. It was differentiated between triple osteotomies exclusively and triple osteotomies combined with a femoral osteotomy (Tab. 8). Pseudarthroses were found in only 4.4%, mainly at the pubis (Tab. 9). In total, embolism was noted in only 1.2% (Tab. 10), thrombosis in 6.4% (Tab .11). Lesions of the sciatic nerve in triple osteotomy alone are listed with 2.1%, but with additional femoral osteotomy in 4.8% (Tab. 12). Most of the lesions recovered to a great extent. In the early follow-up we found only 1.8% peroneal palsies (n=216). An increased Trendelenburg limp was seen in 4%.
| TPO | 188 |
|---|---|
| TPO + FO | 63 |
| Total | 251 |
| Localization | n | % | Total |
|---|---|---|---|
Os pubis |
8 |
||
Os ilium |
2 |
||
Pubis + Illium |
1 |
||
Femur |
0 |
||
Total |
11 |
4.4 |
251 |
| Operation | n | % | Total |
|---|---|---|---|
TPO |
2 |
1,1 |
188 |
TPO + FO |
1 |
1,6 |
63 |
Total |
3 |
1,2 |
251 |
| Operation | n | % | Total |
|---|---|---|---|
TPO |
12 |
6,4 |
188 |
TPO + FO |
4 |
6,4 |
63 |
Total |
16 |
6,4 |
251 |
| Sciatic nerve | n | % | Total |
|---|---|---|---|
TPO |
4 |
2,1 |
188 |
TPO + FO |
3 |
4,8 |
63 |
Total |
7 |
2,8 |
251 |
DISCUSSION
In the clinical grading of pain, ability of walking and the patients’ opinion in the first material 85% of the patients were seen in the groups of “good” and “very good”. In our grading of acetabular measurements of normal values and grades of deviation, the centered joints of decentration grade 1 had normal values (grade 1) in 78% (31). The decentered joints of grade 2 showed grade 1 in 51% and grade 2 in 17.9%. But this has improved in the last follow-up of Küpper with more rotation (Fig. 34, 35).
In 82% of 213 there was no increase of osteoarthrosis. In the survivalrate curve with different degrees of pain according to Harris, 49% were free of pain, 43% had only occasional and mild pain, and only 8% showed severe pain. All these findings demonstrate the efficiency of our Triple osteotomy. In the decentration grades 3 and 4 we had a learning curve and the later results were much better with increased rotation and the use of screws.
In the last follow-up of Küpper the material of one year (89%) after 11.5 years was investigated, but only patients with grades 1 and 2 of decentration, osteoarthosis and the Mose degrees 0-2 for non-congruence (Mose 1980). The Harris hip score improved from 60.6 points in average to 89.3 at follow-up. The acetabular measurements, as already mentioned, were almost all in the normal range. 39% of the joints were free of pain. But 51% had slight occasional pain or mild pain. We believe that this is due to a decrease of acetabular and occasionally femoral anteversion which we have not realized at that time. But otherwise the surgical results, we think, are as optimal as they should be.
There are, however, other factors, upon which we do have no influence: the degree of arthrosis of a joint (4, 26, 27) and the loss of sphericity of a femoral head which can be measured by the circles of Mose (19). Joints without arthrosis were free of pain in 70% (Tab. 13) and joints with Mose grade 1 and 2 only, also in 71% (Tab. 4). Therefore treatment should begin when the patient feels regular pain on longer walking, not with the appearance of osteoarthrosis.
| Grade | No Pain (%) | Total |
|---|---|---|
| Grade 0 | 70 |
99 |
| Grade 1 | 56 |
43 |
| Grade 2 | 36 |
22 |
| Grade 3 | 20 |
5 |
| Mose Grade | No Pain (%) | Total |
|---|---|---|
normal (0-1) |
71 |
97 |
pathological (>1) |
45 |
69 |
The rate of complications was very low. Care should be taken not to traumatize the sciatic nerve, especially if femoral osteotomies are performed additionally. The sciatic nerve should not be extended after the femoral osteotomy. At the ischial osteotomy the nerve should be left covered by the muscles. Double curved retractors are safer than sharpedged.
New methods create new problems and stimulate again new methods. We have changed the approach and the technique of the ilium osteotomy as described in the chapter of “Present technique of triple pelvic osteotomy.” The ilium osteotomy is now performed from the inner side of the pelvis. Therefore the medial glutaeus muscle is not traumatized and also the blood vessels of the lateral side of the pelvic wing. The osteotomy with a curve of an angle of 90° was also introduced, because it spared the number of bone chips, which we brought usually into the gap of the osteotomy.
Different indications and possibilities of triple pelvic osteotomy
Finally some pictures should show our indications and possibilities in unusual deformations. Patients with coxa vara frequently have only little or no abduction. Triple osteotomy then is not possible, unless we perform a valgus osteotomy of the femur before. This is seen in Fig. 37-38 and also our technique to medialize the joint to reduce the load.
 Fig. 37: Severely deformed hip joint with an elongated acetabulum and a sort of secondary acetabulum. Coxa vara is present and abduction very limited. Lateral acetabular rotation therefore is not possible.
Fig. 37: Severely deformed hip joint with an elongated acetabulum and a sort of secondary acetabulum. Coxa vara is present and abduction very limited. Lateral acetabular rotation therefore is not possible.
 Fig. 38: In cases like this one, after a valgus osteotomy the femoral head practically can take the acetabulum with it in a lateral rotation. The femoral head now is well covered.
Fig. 38: In cases like this one, after a valgus osteotomy the femoral head practically can take the acetabulum with it in a lateral rotation. The femoral head now is well covered.
Deformed femoral heads after Perthes disease can also be covered by triple osteotomy (Fig. 39-40). When the greater trochanter is placed more lateral and a bit distally, the femoral neck gets longer and as well the lever arm for the muscles.
 Fig. 39: Deformed hips and dislocated femoral heads after Perthes disease.
Fig. 39: Deformed hips and dislocated femoral heads after Perthes disease.
 Fig. 40: Triple pelvic osteotomy achievs here a good acetabular coverage. When the greater trochanter is placed more lateral and a bit more distally the femoral neck gets longer and as well the lever arm for the muscles.
Fig. 40: Triple pelvic osteotomy achievs here a good acetabular coverage. When the greater trochanter is placed more lateral and a bit more distally the femoral neck gets longer and as well the lever arm for the muscles.
In Fig. 41 we have a similar situation in a 26 year old women. A flattened femoral head is seen, only half covered, and the teardrop figure deeply underneath, greater trochanter high and very close. The trochanter was transplanted lateral and distally (Fig. 42). The femoral head then was covered congruently. The teardrop figure appears now in a normal position.
 Fig. 41: A similar finding as in Fig. 33, but in a 26 year old women.The flattened femoral head is only half covered. Greater trochanter high and very close, limiting abduction and lateral acetabular rotation.
Fig. 41: A similar finding as in Fig. 33, but in a 26 year old women.The flattened femoral head is only half covered. Greater trochanter high and very close, limiting abduction and lateral acetabular rotation.
 Fig. 42: After transplantation of the trochanter lateral and distally the lateral acetabular rotation was possible and effective.
Fig. 42: After transplantation of the trochanter lateral and distally the lateral acetabular rotation was possible and effective.
Dysplasia of the hip in a 10 year old girl with coxa valga is seen in Fig. 43. The pressure of the femoral head is directed against the lateral acetabular rim. Therefore the cartilagenous growth centers are developing an os acetabuli. Triple osteotomy covered the femoral head and centered the pressure into the acetabulum. Fig. 44 shows the growth of the acetabulum after 5 years. Apparently the growth centers were relieved from pressure right in time.
 Fig. 43: Dysplasia of the left hip in a 10 year old girl. The pressure of the femoral head with coxa valga is preventing the growth of the acetabular rim.
Fig. 43: Dysplasia of the left hip in a 10 year old girl. The pressure of the femoral head with coxa valga is preventing the growth of the acetabular rim.
 Fig. 44: 5 years after triple osteotomy the radiography proves that the cartilaginous growth centers had then functioned well.
Fig. 44: 5 years after triple osteotomy the radiography proves that the cartilaginous growth centers had then functioned well.
The two last patients have the longest follow-up of 24 years, the first with a joint of the optimal low decentration grade 1, and the second with a false joint (decentration grade 3). The first patient (Fig. 45-46) was an airline-pilot whom we operated in 1982 at the age of 25. For 24 years he was free of pain and working as captain of long range flights. His sports were tennis, golf and occasionally mountain climbing.
 Fig. 45: Developmental hip dysplasia in an airline pilot 25 years of age. Decentration grade 1, but CE angle only 3° and angle of the weight bearing zone 30°.
Fig. 45: Developmental hip dysplasia in an airline pilot 25 years of age. Decentration grade 1, but CE angle only 3° and angle of the weight bearing zone 30°.
 Fig. 46: 24 years after triple pelvic osteotomy the patient is free of pain, and still very sportive and captain of long-distance flights. Measurements of the hip are normal. No signs of osteoarthrosis.
Fig. 46: 24 years after triple pelvic osteotomy the patient is free of pain, and still very sportive and captain of long-distance flights. Measurements of the hip are normal. No signs of osteoarthrosis.
The woman of Fig. 47-49 had a congenital hip dislocation. The mother took Thalidomid. At the age of 9 years a Chiari osteotomy was performed and the false joint developed astonishingly. But the weight bearing area was too small and pain was present at 18 years. Then we performed a triple pelvic osteotomy. The joint space was normal then and the coverage horizontal, but the weight bearing area of course somewhat shorter than normal. 15 years she was completely free of pain, although she had a farm and heavy work with vegetables, fruits and flowers. Pain developed slowly and became heavy in the last two years. She received a total hip now after 24 years at the age of 42 years.

Fig. 47: Preoperative picture after congenital hip dislocation and a Chiari osteotomy at the age of 9 years. The right hip has a false joint with a small weight bearing zone with a higher angle.

Fig. 48: At 18 years a triple osteotomy was performed. The coverage was horizontal then, the joint space high and normal.

Fig. 49: After 24 years and heavy work on a farm the joint space is worn off because the weight bearing area was too small. She received a total hip now. 15 years she was free of pain, then felt it slowly increasing.
Conclusions
From our results we come to the following conclusions:
- In this type of acetabular redirection all three osteotomies are performed under direct vision and two are controlled also with the image intensifier.
- The ilium osteotomy, performed from the inner side of the pelvic wing, does not traumatize the medial gluteus muscle and the external vascular supply of the pelvis.
- The acetabulum can be rotated extremely, so far that the lateral part of the osteotomized pubis can overlap the medial part, as far as necessary for a horizontal weight bearing surface (Fig. 7-8, Fig. 9-10). Our osteosynthesis, first by wire cerclage, now by screws, avoids pseudarthroses and gives more stability.
- Future vaginal deliveries are preserved (Küpper 2002). The edges of the lateral pubic bone disappear in time.
- Patients can walk on crutches without weight bearing after a few days.
- The joint measurements of the decentration grades 1 and 2 postoperatively, in the 11.5 year follow-up of 1988 (Küpper 2002), are practically always found at normal values. In the false joints and high dislocated (grades 3 and 4) we also achieve good and fair results today.
- Good long-time results can be expected as the two last figures show. When the decrease of acetabular and femoral anteversion pre- and postoperatively will be more diagnosed and corrected in the future, early remissions of moderate pain, as so far observed, will also be less. Anterior rotation of the acetabulum has always to be connected with internal rotation up to a normal acetabular anteversion of 15-20°. A normal internal range of movement should always be checked at 45° of flexion and be present at the end of operation.
- This type of osteotomy is indicated in children when transiliac osteotomies (Tönnis 1984, 1987, 1993, Tönnis et al. 1994) are not suffcient or the child is older than 10-12 years. Triple osteotomies should be performed when pain is felt regularly at longer walks. The development of osteoarthrosis should be avoided because the long time results will be less good then (Bloch 1994, Tönnis et al. 1998).
In the introduction we described already the different rotational osteotomies of the acetabulum and their problems.
Our triple pelvic osteotomy is mainly performed in Germany and adjoining countries. Very positive reports were given by Kirschner et al. (2002), Tschauner et al. (1992), Kleuver et al (1997) and Kooijman et al.(1990). In France the similar osteotomy of Carlioz (Carlioz et al. 1982) is preferred, in Switzerland and the USA the periacetabular osteotomy of Ganz (Ganz et al.1988).
When asked, why we prefer our type of triple osteotomy, we criticize in the osteotomy of Carlioz that he osteotomizes the ischium below the ischial spine, transversely, close to the ischial tuberosity, Then the sacroischial ligament stays on the acetabulum and will not allow extreme rotations. And a cleft is left here, while in our oblique osteotomy the contact of the ischial osteotomysurfaces is remaining.
Opposite to the periacetabular osteotomy of Ganz our three osteotomies are superficially and clearly visible to the eye and the image intensifier. The periacetabular osteotomy is performed deep in the hip, very close to the surface of the joint and its vascular system. Avascular necroses are possible. And it would be interesting to know whether joints with osteoarthrosis grade 2 or 3, whom we operate when they are younger and not too heavy, have a good result. We prefer also the osteosythesis of the pubis osteotomy, especially when we rotate exstremely. When patients had a pseudarthrosis, and even with not much pain, and they were operated and stabilized, they all felt better and preferred it.
Another difference is that our osteotomies do not interfere with the triradiate cartilage zone of children as the periacetabular osteotomy does. Therefore, when triple osteotomies are prefered in children with Perthes disease instead of acetabuloplasties, there is no problem (Fig. 39-40).
REFERENCES
- Anda S., Svenningsen S., Grontvedt T., Benum P, (1990), Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computed tomographic and clinical investigation. Acta Radiol., 31:389-494
- Bloch M. (1994), Untersuchung praeoperativer und operativer Einflußfaktoren auf die Spätergebnisse der Dreifach-Beckenosteotomie nach Tönnis. Inaugural-Dissertation, University of Münster, Germany
- Bombelli R., Santore R.F., Poss R. (1984), Mechanics of the normal and osteoarthritic hip. A new perspective. Clin. Orthop., 182:69-78
- Busse J., Gasteiger W., Tönnis D. (1972), Eine neue Methode zur röntgenologischen Beurteilung eines Hüftgelenkes - der Hüftwert. Arch. Orthop. Trauma Surg, 72:1-9
- Carlioz H., Khouri N., Hulin P. (1982), Osteotomie triple juxtacotiloidienne. Rev. Chir. Orthop., 68:497-501
- Eppright R.H. (1975), Dial osteotomy in the treatment of dysplasia of the hip. In: Proceedings of the American Orthopaedic Association. J. Bone Joint Surg., Am 57:1172
- Ganz R., Klaue K., Vinh T.S., Mast J.W. (1988), A new periacetabular osteotomy for the treatment of hip dysplasia. Technique and preliminary results. Clin. Orthop ,232:26-36
- Harris W. H. (1969), Traumatic arthritis of the hip after dislocation and acetabular fractures. Treatment by mold arthroplasty. J Bone Joint Surg., Am 51: 737-755
- Hopf (1966), Hüftpfannenverlagerung durch doppelte Beckenosteotomie zur Behandlung der Hüftdysplasie und Subluxation bei Jugendlichen und Erwachsenen. Z. Orthop., 101:55-86
- Katthagen B.D., Kalchschmidt K., Tönnis D. (2001), Complications and technical failures of triple pelvic osteotomy. 21. Annual Meeting of European Pediatric Orthopaedic Society, Montpellier
- Kirschner S., Raab P., Wild A., Krauspe R. (2002), Clinical and radiological short- and mid-term results of triple osteotomy according to Tönnis in adolescents and adults. Z. Orthop., 140:523.526
- Kleuwer M., Kooijman M.A.P., Pavlov P.W., Veth R.P.H. (1997), Triple osteotomy of the pelvis for acetabular dysplasia, Results at 8 to 15 years. British Editorial Society of Bone and Joint Surgery, 79B: 225-229
- Kooijman M.A.P., Pavlov P. (1990), Triple osteotomy of the pelvis. A review of 51 cases. Clin. Orthop., 255:133-137
- Küpper A. (2002), Mittelfristige Ergebnisse der dreifachen Beckenosteotomie nach Tönnis. Eine klinische und radiologische Nachuntersuchung nach 11,5 Jahren. Inaugural-Dissertation, University of Gießen, Germany
- Le Coer P. (1965), Correction des défauts d`orientation de l`isthme iliaque. Rev. Chir. Orthop., 51:211-212
- Lequesne M., de Seze S. (1961), Le faux profil du bassin. Nouvelle incidence radiographique pour l`ètude de la hanche. Rev. Rhum. Mal. Osteoartic, 28:643-652
- Lingg G., von Torklus D. (1981), Röntgenzeichen der azetabulären Hüftdysplasie bei Erwachsenen. Radiologe, 21:291-295
- Millis M.B., Murphy S.B. (1998), The Boston concept. Periacetabular osteotomy with simultaneous arthrotomy via direct anterior approach. Orthopäde, 27:751-758
- 19. Mose K. (1980), Methods of measuring in Legg-Calvé-Perthes disease with special regard to the prognosis. Clin . Orthop., 150:103-109
- Murphy S.B., Millis M.B. (1999), Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin. Orthop., 364:92-98
- Reimers J. (1980), The stability of the hip in children. Acta Orthop. Scand., suppl: 184
- Severin E. (1941), Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed and arthrographic studies of recent cases. Acta Chir. Scand., 64:suppl 63
- Steel H.H. (1973), Triple-osteotomy of the innominate bone. J. Bone Joint Surgery, Am 55:343-350
- Sutherland D.H., Greenfield R. (1974), Double innominate osteotomy. J. Bone Joint Surg., Am 59:1082-1090
- Tönnis D. (1976), An evaluation of conservative and operative methods in the treatment of congenital hip dislocation. Clinical Orthop., 119:76-88
- Tönnis D. (1984), Die angeborene Hüftdysplasie und Hüftluxation im Kindes- und Erwachsenalter. Springer, Heidelberg, pp 309-321
- Tönnis D. (1987), Congenital dysplasia and dislocation of the hip in children and adults. Springer Berlin, Heidelberg, New York, pp 370-381
- Tönnis D., Behrens K., Tscharani (1981), A modified technique of triple osteotomy. J. Pediatr. Orthop., 1:241-249
- Tönnis D., Behrens K., Tscharani (1981), Eine neue Technik der Dreifachosteo- tomie zur Schwenkung dysplastischer Hüftpfannen bei Jugendlichen und Erwachsenen. Z. Orthop., (1981) 119:253-263
- Tönnis D. (1993), Treatment of residual dysplasia after developmental dysplasia of the hip as a prevention of early coxarthrosis. J. Pediatr. Orthop., part B, 2:133-144 (available only in libraries)
- Tönnis D., Arning A., Bloch M., Heinecke A., Kalchschmidt K. (1994), Triple pelvic osteotomy. J. Pediatr. Orthop. part B, 3:54-67 (available only in libraries)
- Tönnis D., Brüning K., Heinecke A., Lateral acetabular osteotomy. J. Pediatr. Orthop., part B (1994), 3:40-46. (available only in libraries)
- Tönnis D., Heinecke A. (1999), Current Concepts Review. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J. Bone. Joint Surg., Am 81:1747-1770
- Tönnis D., Heinecke A. (1999), Verringerte Pfannenanteversion und Schenkelhalsantetorsion verursachen Schmerz und Arthrose. Z Orthop. 137 part 1: Statistik und klinische Folgen: 153-159. part 2: Ätiologie, Diagnostik und Therapie: 160-167
- Tönnis D., Skamel H.J. (2003), Besonderheiten bei der Bestimmung der Hüftpfannenanteversion und Schenkelhalsantetorsion durch Computertomographie. Radiologe 43:735-739
- Tönnis, D., Kalchschmidt K., Heinecke A. (1998), Hüftpfannenschwenkung durch Dreifachosteotomie des Beckens nach Tönnis. Orthopäde 27:733-742 37. Tschauner C, Klapsch W, Kohlmeier W, Graf R (1992) Die dreifache Beckenosteotomie nach Tönnis im Rahmen der Spätdysplasie und Sekundärarthrose des Hüftgelenkes. Orthop. Prax., 28:255-263
- Visser J.D., Jonkers A. (1980), A method for calculating acetabular anteversion, femur anteversion and the instability index of the hip joint. Netherlands J. Surg. 32:146-149
- Wiberg G. (1939), Studies on dysplastic acetabulum and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta. Chir. Scand., 83:suppl 58
- Wiberg G. (1953), Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J. Bone Joint Surg., Am 35:65-68
| Download | |
|---|---|
| Update of Triple Pelvic Osteotomy | PDF (884 KB) |